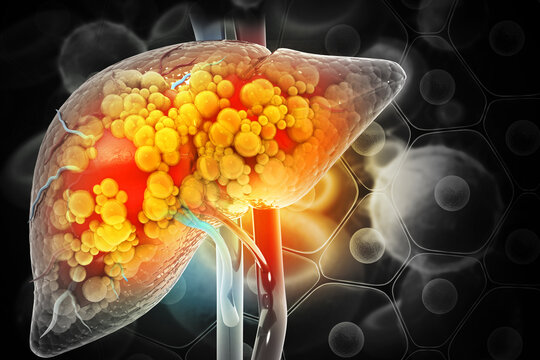
Fatty Liver Disease (वसायुक्त यकृत रोग), also known as Hepatic Steatosis and Steatotic Liver Disease (SLD), is a condition where excess fat builds up in the liver. Complications may include cirrhosis, liver cancer, and esophageal varices. The main subtypes of fatty liver disease (FLD) are Metabolic Dysfunction–Associated Steatotic Liver Disease (MASLD, formerly “Non-Alcoholic Fatty Liver Disease” (NAFLD)) and Alcoholic Liver Disease (ALD), with the category “Metabolic and Alcohol Associated Liver Disease” (metALD) describing an overlap of the two. The primary risks include alcohol, type 2 diabetes, and obesity. Treatment of NAFLD typically involves dietary changes and exercise to promote weight loss. In those who are severely affected, liver transplantation may be an option. More than 90% of heavy drinkers develop fatty liver, while about 25% develop the more severe alcoholic hepatitis.
Fatty Liver Disease Meaning
Fatty Liver Disease refers to a medical condition where excess fat accumulates in the liver cells. Normally, the liver contains some fat, but when more than 5%–10 % of the liver’s weight is fat, it is considered a fatty liver. This buildup can interfere with liver function and may lead to inflammation, scarring, or serious complications if not managed.
Risk Factors of Fatty Liver Disease
Fatty Liver Disease (FLD) develops when fat accumulates in liver cells due to various metabolic, lifestyle, or environmental factors. These risk factors increase the chances of developing either Non-Alcoholic Fatty Liver Disease (NAFLD) or Alcoholic Fatty Liver Disease (AFLD).
Major Risk Factors
Obesity
-
The most common risk factor for NAFLD.
-
Excess body fat, especially abdominal obesity, increases fat deposits in the liver.
Type 2 Diabetes & Insulin Resistance
-
High insulin levels cause fat to build up in the liver.
-
NAFLD is highly prevalent in people with diabetes.
Poor Diet
-
High intake of:
-
Refined sugars (fructose, corn syrup)
-
Saturated fats
-
Junk or processed foods
-
-
Low intake of:
-
Fiber
-
Fruits and vegetables
-
High Cholesterol & Triglycerides
-
Elevated blood lipids contribute to liver fat buildup.
Alcohol Consumption
-
A major cause of Alcoholic Fatty Liver Disease (AFLD).
-
Even moderate drinking can worsen fatty liver in vulnerable individuals.
Physical Inactivity
Age and Gender
-
Risk increases with age.
-
Men are more prone to AFLD; postmenopausal women may be more vulnerable to NAFLD.
Genetic and Family History
-
Genetic variations (e.g., PNPLA3 gene mutation) may raise susceptibility.
-
A family history of liver disease or metabolic disorders increases risk.
Certain Medications
-
Examples: corticosteroids, tamoxifen, methotrexate, amiodarone.
-
May trigger or worsen liver fat accumulation.
Other Medical Conditions
-
Polycystic ovary syndrome (PCOS)
-
Metabolic syndrome
Summary Chart
| Risk Factor | Affects |
|---|---|
| Obesity | Metabolism & fat storage |
| Type 2 Diabetes | Insulin resistance |
| Alcohol intake | Liver metabolism (AFLD) |
| Poor diet | Triglyceride production |
| Lack of exercise | Fat burn and insulin sensitivity |
| High cholesterol/triglycerides | Liver fat synthesis |
| Genetic predisposition | Liver fat storage & inflammation |
Fatty Liver Disease Classification
Fatty Liver Disease (FLD), also known as hepatic steatosis, is classified into two main types based on the cause and underlying factors:
Non-Alcoholic Fatty Liver Disease (NAFLD)
This is the most common type, especially in people who drink little or no alcohol. It is associated with metabolic risk factors.
Subtypes of NAFLD
-
Simple Fatty Liver (Steatosis)
-
Fat accumulates in the liver without inflammation or liver cell damage.
-
Generally considered benign and reversible.
-
-
Non-Alcoholic Steatohepatitis (NASH)
-
Involves fat buildup along with inflammation and liver cell damage.
-
Can progress to fibrosis, cirrhosis, or liver cancer.
-
Risk Factors
-
Obesity
-
Type 2 diabetes
-
High cholesterol or triglycerides
-
Metabolic syndrome
-
Sedentary lifestyle
Alcohol-Associated Fatty Liver Disease (AFLD)
Also called Alcoholic Fatty Liver Disease, this form results from excessive alcohol consumption.
Subtypes of AFLD
-
Alcoholic Fatty Liver (Simple Steatosis)
-
Fat accumulates in liver cells due to heavy alcohol intake.
-
Reversible with abstinence.
-
-
Alcoholic Steatohepatitis (ASH)
-
Involves inflammation and liver damage due to alcohol.
-
May progress to fibrosis and cirrhosis if alcohol use continues.
-
Risk Factors
-
Chronic heavy alcohol consumption
-
Genetic predisposition
-
Poor nutrition
-
Coexisting liver diseases (e.g., hepatitis C)
Special Forms / Related Conditions
-
Acute Fatty Liver of Pregnancy (AFLP)
-
Rare but serious condition in late pregnancy.
-
Requires immediate medical attention.
-
-
Drug-Induced Fatty Liver
-
Caused by certain medications (e.g., corticosteroids, methotrexate, amiodarone).
-
-
Lipid Storage Diseases (rare genetic conditions)
-
Such as Gaucher disease or Niemann–Pick disease.
-
Comparison Table: Types of Fatty Liver Disease
| Type | Subtypes | Causes | Key Features | Risk Factors | Reversibility |
|---|---|---|---|---|---|
| Non-Alcoholic Fatty Liver Disease (NAFLD) | – Simple Steatosis – Non-Alcoholic Steatohepatitis (NASH) |
Metabolic syndrome, insulin resistance | Fat in liver without (or with) inflammation and damage | Obesity, Type 2 diabetes, and high cholesterol | Yes (especially early stages) |
| Alcoholic Fatty Liver Disease (AFLD) | – Alcoholic Steatosis – Alcoholic Steatohepatitis (ASH) |
Chronic alcohol intake | Fat accumulation, liver inflammation, and cell damage | Heavy drinking, poor diet, and genetics | Yes, if alcohol is stopped early |
| Acute Fatty Liver of Pregnancy (AFLP) | N/A | Pregnancy-related metabolic dysfunction | Rapid liver failure symptoms in late pregnancy | Third trimester of pregnancy | Requires urgent delivery; often reversible |
| Drug-Induced Fatty Liver | N/A | Certain medications (e.g., steroids, chemo) | Fat deposition from toxic drug effects | Long-term medication use | Often reversible if drugs are stopped |
| Inherited Fat Storage Disorders | Gaucher, Niemann-Pick, etc. | Genetic mutations | Abnormal fat storage in the liver and other organs | Family history, genetic mutations | Usually chronic, managed, not cured |
Fatty Liver Disease Symptoms
Fatty Liver Disease (FLD) often exhibits no symptoms in the early stages, particularly in simple steatosis (fat accumulation without inflammation). However, as the disease progresses, especially to NASH (Non-Alcoholic Steatohepatitis) or ASH (Alcoholic Steatohepatitis), symptoms may begin to appear.
Common Symptoms of Fatty Liver Disease
-
Often asymptomatic
-
May be found incidentally on imaging or blood tests
-
Moderate Stage (NASH or ASH) |
-
Fatigue or weakness
-
Mild pain or discomfort in the upper right abdomen
-
Unexplained weight loss
-
Loss of appetite
-
Enlarged liver (hepatomegaly)
Advanced Stage (Fibrosis or Cirrhosis)
-
Abdominal swelling (ascites)
-
Yellowing of the skin or eyes (jaundice)
-
Itchy skin
-
Swelling in the legs and ankles
-
Spider-like blood vessels on the skin
-
Confusion or difficulty concentrating (hepatic encephalopathy)
-
Easy bruising or bleeding
Associated Lab or Clinical Findings
-
Elevated liver enzymes (ALT, AST)
-
Elevated GGT (in AFLD)
-
Abnormal liver ultrasound or MRI
-
Liver biopsy (to confirm NASH or fibrosis)
Fatty Liver Disease Causes
The causes of Fatty Liver Disease (FLD) differ based on its two main types: Non-Alcoholic Fatty Liver Disease (NAFLD) and Alcoholic Fatty Liver Disease (AFLD). However, the common feature in all cases is the excess accumulation of fat in liver cells.
Non-Alcoholic Fatty Liver Disease (NAFLD) – Causes
Occurs in people who consume little or no alcohol. It’s closely linked to metabolic disorders.
| Cause | Explanation |
|---|---|
| Obesity | Increases fat storage in liver cells. Central/abdominal obesity is especially risky. |
| Type 2 Diabetes | Insulin resistance promotes fat buildup in the liver. |
| High Blood Lipids | Elevated triglycerides or LDL cholesterol contribute to fat accumulation. |
| Metabolic Syndrome | A cluster of conditions (obesity, high BP, high sugar, high cholesterol) that raises liver fat. |
| Sedentary Lifestyle | Lack of exercise reduces fat metabolism and worsens insulin resistance. |
| Poor Diet | High intake of sugar, refined carbs, and saturated fats increases liver fat. |
| Rapid Weight Loss or Malnutrition | It can paradoxically lead to fat mobilization to the liver. |
| Genetics and Ethnicity | Family history and being of Hispanic or South Asian descent raise risk. |
| Certain Medications | Long-term use of corticosteroids, tamoxifen, methotrexate, etc. |
Alcoholic Fatty Liver Disease (AFLD) – Causes
Caused by chronic excessive alcohol consumption.
| Cause | Explanation |
|---|---|
| Heavy Alcohol Use | Alcohol impairs fat metabolism, leading to the accumulation of triglycerides in liver cells. |
| Poor Nutrition in Alcoholics | Deficiencies in protein and vitamins make the liver more vulnerable. |
| Genetics | Some people are genetically more susceptible to alcohol-related liver damage. |
| Other Liver Stressors | Hepatitis C, co-use of liver-toxic medications, or repeated binge drinking. |
Other Specific Causes
| Cause | Context |
|---|---|
| Acute Fatty Liver of Pregnancy (AFLP) | A rare, serious liver disorder that occurs in late pregnancy due to mitochondrial dysfunction. |
| Drug-Induced Liver Injury | Caused by medications like amiodarone, valproate, and tamoxifen. |
| Genetic Lipid Storage Disorders | Such as Gaucher’s disease or Niemann–Pick disease. |
Fatty Liver Disease Diagnosis
Fatty Liver Disease (FLD) is diagnosed using a combination of clinical evaluation, lab tests, and imaging studies, and sometimes confirmed through a liver biopsy.
Medical History & Physical Examination
-
History Taking
-
Alcohol consumption habits
-
Metabolic conditions (obesity, diabetes, high cholesterol)
-
Medication use
-
Family history of liver disease
-
-
Physical Exam
-
May show an enlarged liver (hepatomegaly)
-
Signs of advanced liver disease (e.g., jaundice, ascites) in late stages
-
Blood Tests (Liver Function Tests & Metabolic Profile)
| Test | Purpose |
|---|---|
| ALT, AST (Liver Enzymes) | Elevated levels suggest liver inflammation or damage |
| GGT & ALP | May also be raised in fatty liver |
| Bilirubin | Increase in advanced liver disease |
| Lipid Profile | Checks cholesterol and triglycerides |
| Fasting Glucose & HbA1c | To detect diabetes or insulin resistance |
| CBC, INR, Albumin | To evaluate overall liver function |
Imaging Tests
| Test | Details |
|---|---|
| Ultrasound | Most common initial test, shows a bright or “fatty” liver |
| CT Scan or MRI | More detailed imaging to assess fat content and liver structure |
| Transient Elastography (FibroScan) | Measures liver stiffness to detect fibrosis or cirrhosis noninvasively |
| MRI-PDFF (Proton Density Fat Fraction) | A specialized MRI technique to quantify liver fat accurately |
Liver Biopsy (If Needed)
-
Gold standard for diagnosing NASH and assessing inflammation or fibrosis.
-
Involves removing a small piece of liver tissue for microscopic examination.
-
Used when:
-
Diagnosis is unclear
-
Suspected NASH or advanced fibrosis
-
Ruling out other liver diseases
-
Additional Tests (To Rule Out Other Conditions)
-
Viral Hepatitis Panel (HBV, HCV)
-
Autoimmune liver disease markers
-
Iron studies (for hemochromatosis)
-
Alpha-1 antitrypsin, ceruloplasmin (for rare liver disorders)
Fatty Liver Disease Treatment
The treatment of Fatty Liver Disease (FLD) primarily focuses on reversing liver fat accumulation, preventing progression, and managing underlying conditions. There are no specific medications approved for FLD in most cases, but lifestyle changes are the cornerstone of treatment.
Lifestyle Modifications (Most Effective)
| Strategy | Details |
|---|---|
| Weight Loss | The most effective treatment for NAFLD. Losing 7–10% of body weight can reduce liver fat and inflammation. |
| Healthy Diet | Adopt a Mediterranean diet: rich in vegetables, fruits, whole grains, nuts, olive oil, and lean protein. Avoid sugar, refined carbs, and processed foods. |
| Regular Exercise | At least 150–300 minutes of moderate exercise per week (e.g., brisk walking, cycling). Helps improve insulin sensitivity and reduce fat. |
| Avoid Alcohol | Essential in AFLD. Even small amounts can worsen liver damage. In NAFLD, alcohol should be minimized or avoided. |
| Control Diabetes & Blood Pressure | Proper management of blood sugar, BP, and cholesterol reduces liver strain. |
Medications (Supportive & In Specific Cases)
| Medication | Used For |
|---|---|
| Vitamin E (800 IU/day) | Antioxidants may help reduce liver inflammation in non-diabetic NAFLD patients. |
| Pioglitazone (Actos) | A diabetes medication may help in NASH with insulin resistance (not for all). |
| GLP-1 agonists (e.g., Semaglutide) | Shown to reduce liver fat and assist with weight loss (emerging therapy). |
| Statins | Safe in NAFLD; used to treat high cholesterol and reduce cardiovascular risk. |
| SGLT2 inhibitors or Metformin | It may help diabetic patients with NAFLD. |
| Pentoxifylline / Obeticholic acid (under study) | Investigational drugs for NASH and fibrosis. |
Note: Always use medications under medical supervision; some can worsen liver disease.
Surgical or Interventional Treatments (If Needed)
| Option | Purpose |
|---|---|
| Bariatric Surgery | For obese individuals who fail lifestyle interventions, it helps reduce liver fat and improve NASH. |
| Liver Transplant | Final option for end-stage liver disease or cirrhosis due to NAFLD or AFLD. |
Supportive & Complementary Approaches
| Method | Benefit |
|---|---|
| Ayurveda/Homeopathy | Some herbs like kutki, bhumyamalaki, and turmeric are traditionally used (more research needed). |
| Behavioral Counseling | Helps with diet, alcohol cessation, and lifestyle change. |
| Vitamin D & Omega-3s | Sometimes recommended to support metabolic health. |
What to Avoid
-
Alcohol
-
Sugar-sweetened beverages
-
Fried and fast food
-
Sedentary lifestyle
-
Self-medicating with herbal products not prescribed by professionals
Natural Remedies for Fatty Liver Disease
Natural remedies for Fatty Liver Disease (FLD) can support liver health, especially in early-stage NAFLD (non-alcoholic fatty liver disease), when combined with medical advice and lifestyle changes. These remedies focus on improving liver detoxification, reducing inflammation, and enhancing metabolism.
Diet-Based Remedies
| Natural Food | Benefits |
|---|---|
| Garlic | Promotes fat breakdown and reduces liver fat levels. |
| Green Tea | Contains antioxidants (catechins) that reduce liver fat and inflammation. |
| Turmeric (Curcumin) | Anti-inflammatory and antioxidant; protects liver cells. |
| Leafy Greens (Spinach, Kale) | High in antioxidants and chlorophyll, which aid detoxification. |
| Beetroot | Supports liver detox and bile production. Rich in betaine. |
| Fatty Fish (like Salmon) | High in omega-3s, which reduce liver fat and improve lipid profile. |
| Avocados | Rich in healthy fats and antioxidants, it may help reduce liver stress. |
Herbal Remedies (Ayurvedic & Traditional)
| Herb | Action on Liver |
|---|---|
| Milk Thistle (Silymarin) | Powerful liver protector; regenerates liver tissue. |
| Kutki (Picrorhiza kurroa) | Classic Ayurvedic liver tonic; detoxifies and strengthens the liver. |
| Bhumyamalaki (Phyllanthus niruri) | Traditionally used for liver disorders; supports liver repair. |
| Guduchi (Tinospora cordifolia) | Reduces liver inflammation and boosts immunity. |
| Amla (Indian Gooseberry) | Rich in vitamin C and antioxidants, it promotes liver health. |
| Licorice Root | Has hepatoprotective and anti-inflammatory effects. |
Note: Always consult an Ayurvedic or naturopathic expert before taking herbal remedies, especially with other medications.
Lifestyle and Mind-Body Practices
| Practice | How It Helps |
|---|---|
| Yoga (e.g., Pawanmuktasana, Dhanurasana, Naukasana) | Improves digestion, reduces belly fat, and stimulates liver function. |
| Pranayama (Anulom Vilom, Bhastrika) | Boosts oxygen supply and supports detoxification. |
| Daily Walking / Moderate Exercise | Enhances fat metabolism and reverses liver fat. |
| Adequate Sleep | Essential for hormone balance and liver regeneration. |
Natural Liver Detox Drinks
| Drink | Ingredients |
|---|---|
| Warm Lemon Water (morning) | Lemon + warm water – stimulates bile and digestion. |
| Amla Juice | Fresh amla or diluted concentrate in water supports liver function. |
| Aloe Vera Juice | Soothes digestion and helps cleanse the liver. |
| Turmeric Milk | Turmeric + warm milk or plant-based milk – anti-inflammatory liver support. |
Supplements (with Natural Origins)
(Use with healthcare supervision)
-
Vitamin E (natural sources like sunflower seeds, almonds)
-
Probiotics (improve gut health and reduce liver inflammation)
-
Vitamin D (deficiency is linked to NAFLD)
Important Notes
-
Natural remedies support but do not replace medical treatment.
-
Always consult a doctor before starting herbs, especially if you have diabetes, are on medications, or are pregnant.
-
Remedies are most effective when combined with lifestyle changes, such as:
-
Losing weight
-
Avoiding alcohol
-
Reducing sugar and processed food
-
Ayurveda Treatments for Fatty Liver Disease
Ayurveda approaches Fatty Liver Disease (Yakrit Roga or Medoroga) as an imbalance primarily of Pitta and Kapha doshas, often influenced by Ama (toxins) and impaired Agni (digestive fire). The focus of Ayurvedic treatment is to restore liver function, balance metabolism, remove toxins, and rejuvenate the liver tissue.
Herbal Formulations (Aushadhi Chikitsa)
| Herb / Formula | Properties & Actions |
|---|---|
| Kutki (Picrorhiza kurroa) | Deep detoxifier and liver stimulant; restores liver enzyme balance. |
| Bhumyamalaki (Phyllanthus niruri) | Excellent for liver regeneration, antiviral, and anti-inflammatory. |
| Guduchi (Tinospora cordifolia) | An immunomodulator helps in detoxifying and rejuvenating the liver. |
| Triphala | Mild laxative and antioxidant; improves digestion and removes Ama. |
| Punarnava (Boerhavia diffusa) | Reduces liver swelling and helps manage fluid retention. |
| Arogyavardhini Vati | Classical formulation for liver, skin, and metabolic disorders. Contains herbs like Triphala, Shuddha Parada, and Loha Bhasma. |
| Liv 52 (Himalaya) | Modern proprietary Ayurvedic medicine to support liver function and fat metabolism. |
| Kalmegh (Andrographis paniculata) | Bitter tonic with strong anti-inflammatory and hepatoprotective actions. |
Panchakarma Therapies (Detoxification Treatments)
| Therapy | Purpose & Benefits |
|---|---|
| Virechana (Therapeutic Purgation) | Main treatment for Pitta disorders. Clears excess fat, toxins, and improves liver metabolism. |
| Basti (Medicated Enema) | Balances Vata and removes deep-seated toxins; used when liver disease is chronic. |
| Abhyanga (Oil Massage) + Swedana (Herbal Steam) | Enhances circulation, reduces Kapha, and supports detox. |
| Shirodhara (Oil dripping on forehead) | Calms the mind and endocrine system, reducing stress-related liver burden. |
Note: Panchakarma should only be done under the supervision of a trained Ayurvedic physician.
Ayurvedic Diet (Ahara) for Fatty Liver
| Recommended Foods | To Avoid |
|---|---|
| Warm, light meals like khichdi, moong dal, steamed vegetables | Fried, spicy, oily, or heavy foods |
| Bitter greens (fenugreek, neem, karela) | Processed food, sugar, and white flour |
| Herbal teas (ginger, cumin, coriander) | Caffeinated or carbonated drinks |
| Fresh fruits like pomegranate, apple | Dairy in excess, red meat, and cheese |
| Use of turmeric, cumin, and coriander in cooking | Cold, raw foods that increase Kapha |
Dinacharya (Daily Routine) & Yoga
| Practice | Effect |
|---|---|
| Wake up early (before sunrise) | Supports liver rhythm and digestion |
| Daily exercise / Yoga (30–45 mins) | Promotes fat metabolism and reduces liver fat |
| Pranayama (Anulom Vilom, Bhastrika) | Detoxifies and improves liver oxygenation |
| Avoid daytime sleeping | Reduces Kapha accumulation |
| Regular bowel movement | Helps eliminate Ama and excess Pitta |
Key Ayurvedic Principles for Fatty Liver Management
-
Balance Agni (digestive fire) with herbs and spices
-
Eliminate Ama (toxins) via Panchakarma and cleansing
-
Pacify Kapha and Pitta doshas
-
Restore Ojas (vitality) and rejuvenate liver tissues (Rasayana therapy)

Fatty Liver Disease Research
A systematic review and meta-analysis published in 2024 found that growth hormone therapy may aid in the management of fatty liver disease.
Conclusion
Fatty Liver Disease (FLD), whether alcoholic or non-alcoholic, is a growing global health concern linked to lifestyle, metabolic disorders, and alcohol consumption. While early stages may be silent, untreated FLD can progress to serious conditions like steatohepatitis, fibrosis, cirrhosis, and even liver cancer.
The encouraging fact is that Fatty Liver Disease is often reversible, especially in its early stages. Timely diagnosis, supported by imaging and lab tests, can lead to effective interventions. Weight management, healthy diet, regular exercise, and abstinence from alcohol remain the most powerful tools in both prevention and treatment. In addition, Ayurvedic and natural remedies, when integrated with modern care and guided by professionals, can provide holistic support to liver healing.
Ultimately, a disciplined lifestyle, personalized care, and regular monitoring can successfully halt the progression of fatty liver and restore liver health, enhancing overall quality of life.
Frequently Asked Questions
Here are 10 Frequently Asked Questions (FAQs) with detailed answers about Fatty Liver Disease (FLD):
What is Fatty Liver Disease?
Fatty Liver Disease (FLD) occurs when excess fat accumulates in liver cells. It has two main types:
-
Non-Alcoholic Fatty Liver Disease (NAFLD): Not related to alcohol use.
-
Alcoholic Fatty Liver Disease (AFLD): Caused by heavy alcohol intake.
What causes Fatty Liver Disease?
Common causes include:
-
Obesity
-
Type 2 diabetes
-
High cholesterol and triglycerides
-
Excessive alcohol consumption (in AFLD)
-
Poor diet and sedentary lifestyle
-
Certain medications and genetic factors
What are the symptoms of Fatty Liver Disease?
Early stages often have no symptoms. In advanced cases, people may experience:
-
Fatigue
-
Discomfort or pain in the upper right abdomen
-
Enlarged liver
-
Unexplained weight loss
-
Jaundice (in severe cases)
How is Fatty Liver Disease diagnosed?
It is usually diagnosed through:
-
Blood tests (liver enzymes like ALT, AST)
-
Imaging (ultrasound, CT scan, MRI)
-
FibroScan (for liver stiffness)
-
Liver biopsy (in uncertain or advanced cases)
Can Fatty Liver Disease be reversed?
Yes. In many cases, especially NAFLD, it is reversible with:
-
Weight loss
-
Healthy diet
-
Regular exercise
-
Avoidance of alcohol
-
Controlling diabetes and cholesterol
What is the difference between NAFLD and AFLD?
-
NAFLD is not caused by alcohol and is linked to metabolic issues like obesity and diabetes.
-
AFLD is directly related to excessive alcohol use.
Is medication required to treat Fatty Liver Disease?
No specific medication is approved universally for FLD. Treatment usually focuses on lifestyle changes. In some cases, doctors may prescribe:
-
Vitamin E (for non-diabetics with NAFLD)
-
Pioglitazone or GLP-1 agonists (for diabetics)
-
Statins (for high cholesterol)
Can Ayurvedic or natural remedies help?
Yes. Herbs like kutki, bhumyamalaki, turmeric, and triphala support liver function. Lifestyle practices such as yoga, pranayama, and a sattvic diet may also help, but should be used under professional guidance and not replace medical care.
What foods should I avoid with Fatty Liver Disease?
Avoid:
-
Fried and processed foods
-
Refined sugars and white bread
-
Alcohol
-
Red meat and full-fat dairy
-
Sugary drinks and sodas
What complications can arise from untreated Fatty Liver Disease?
If left untreated, FLD can progress to:
-
NASH (Non-Alcoholic Steatohepatitis)
-
Fibrosis (scarring)
-
Cirrhosis (advanced liver damage)
-
Liver failure or liver cancer
Reference: https://en.wikipedia.org/wiki/Fatty_liver_disease

