Miscarriage (???????), also known as spontaneous abortion and pregnancy loss, is the natural death of an embryo or fetus before it is able to survive independently. Some use the cutoff of 20 weeks of gestation, after which fetal death is known as a stillbirth. The most common symptom of a miscarriage is vaginal bleeding with or without pain. Sadness, anxiety, and guilt often occur afterward. Tissue and clot-like material may leave the uterus and pass through and out of the vagina. Among women who know they are pregnant, the miscarriage rate is roughly 10% to 20%, while rates among all fertilization are around 30% to 50%. Having this problem a great impact on the woman, Siddha Spirituality of Swami Hardas Life System has a unique method, which can effectively deal with miscarriage and fertility. Hence, let us know everything about miscarriage and learn free Siddha energy remedies.
Miscarriage meaning (??????? ?? ????)
Meaning of miscarriage is an early, unintentional end to a pregnancy when the baby is born too early and dies because it has not developed enough:
Signs & symptoms (????? ?? ?????)
Signs of a miscarriage include:
- Vaginal spotting
- Abdominal pain
- Cramping
- Fluid, blood clots
- Tissue passing from the vagina
Bleeding can be a symptom of miscarriage, but many women also have bleeding in early pregnancy and don’t miscarry. Bleeding during pregnancy may be referred to as a threatened miscarriage.
Risk factors (????? ???)
Miscarriage may occur for many reasons, not all of which can be identified. Risk factors are those things that increase the likelihood of having a miscarriage but don’t necessarily cause a miscarriage. The risk includes up to 70 conditions:
- Infections
- Medical procedures
- Lifestyle factors
- Occupational Exposures
- Chemical exposure
- Shift work
Some of these risks include:
- Endocrine
- Genetic
- Uterine
- Hormonal abnormalities
- Reproductive tract infections
- Tissue rejection caused by an autoimmune disorder
Trimesters (??????)
First trimester (???? ??????)
Most clinically apparent miscarriages occur during the first trimester. About 30% to 40% of all fertilized eggs miscarry, often before the pregnancy is known. The embryo typically dies before the pregnancy is expelled; bleeding into the decidua basalis and tissue necrosis causes uterine contractions to expel the pregnancy.
Early miscarriages can be due to a developmental abnormality of the placenta or other embryonic tissues. In some instances, an embryo does not form but other tissues do. This has been called a “blighted ovum”.
Successful implantation of the zygote into the uterus is most likely 8 to 10 days after conception. If the zygote has not implanted by day 10, implantation becomes increasingly unlikely in subsequent days.
A chemical pregnancy is a pregnancy that was detected by testing but ends in miscarriage before or around the time of the next expected period.
Chromosomal abnormalities are found in more than half of embryos miscarried in the first 13 weeks. Half of the embryonic miscarriages have an abnormal number of chromosomes. Common chromosome abnormalities found in miscarriages include:
- Autosomal trisomy
- Monosomy X
- Triploidy
- Tetraploidy
- Other structural chromosomal abnormalities
Genetic problems are more likely to occur with older parents; this may account for the higher rates observed in older women.
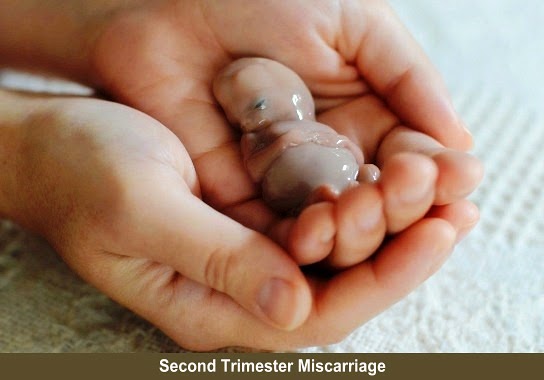
Second and third trimesters (????? ?? ????? ??????)
Second-trimester losses may be due to maternal factors such as:
- Uterine malformation
- Growths in the uterus
- Cervical problems
These conditions also may contribute to premature birth. Unlike first-trimester miscarriages, second-trimester miscarriages are less likely to be caused by a genetic abnormality; chromosomal aberrations are found in a third of cases. Infection during the third trimester can cause a miscarriage.
Age of pregnant woman (??????? ????? ?? ???)
The age of the pregnant woman is a significant risk factor. Miscarriage rates increase steadily with age, with more substantial increases after age 35. In those under the age of 35, the risk is about 10% while it is about 45% in those over the age of 40.
Obesity, eating disorders and caffeine (??????, ???? ?? ????? ?? ?????)
Not only is obesity associated with miscarriage; it can result in sub-fertility and other adverse pregnancy outcomes. Recurrent miscarriage is also related to obesity. Women with bulimia nervosa and anorexia nervosa may have a greater risk for miscarriage.
Caffeine consumption also has been correlated to miscarriage rates, at least at higher levels of intake. However, such higher rates have been found to be statistically significant only in certain circumstances.
Vitamin supplementation has generally not shown to be effective in preventing miscarriage. Chinese traditional medicine has not been found to prevent miscarriage.
Endocrine disorders (?????????? ?????)
Disorders of the thyroid may affect pregnancy outcomes. Related to this, iodine deficiency is strongly associated with an increased risk of miscarriage. The risk of miscarriage is increased in those with poorly controlled insulin-dependent diabetes mellitus. Women with well-controlled diabetes have the same risk of miscarriage as those without diabetes.
Food poisoning (??????? ????)
Ingesting food that has been contaminated with listeriosis, toxoplasmosis, and salmonella is associated with an increased risk of miscarriage.
Amniocentesis and chorionic villus sampling (?????????????? ?? ????????? ???? ?????)
Amniocentesis and chorionic villus sampling (CVS) are procedures conducted to assess the fetus.
Surgery (????????????)
The effects of surgery on pregnancy are not well-known including the effects of bariatric surgery. Abdominal and pelvic surgery are not risk factors in miscarriage. Ovarian tumors and cysts that are removed have not been found to increase the risk of miscarriage.
Medications (?????)
Immunizations have not been found to cause miscarriage. There is no significant association between antidepressant medication exposure and spontaneous abortion.
Some available data suggest that there is a small increased risk of miscarriage for women taking an antidepressant, though this risk becomes less statistically significant when excluding studies of poor quality.
Medicines that increase the risk of miscarriage include:
- Retinoids
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as Ibuprofen
- Misoprostol
- Methotrexate
Chemotherapy and radiation treatments for cancer (????? ?? ??? ?????????? ?? ?????? ?????)
Ionizing radiation levels are given to a woman during cancer treatment cause miscarriage. Exposure can also impact fertility. The use of chemotherapeutic drugs used to treat childhood cancer increases the risk of miscarriage.
Intercurrent diseases (???:?????? ?????????)
Several intercurrent diseases in pregnancy can potentially increase the risk of miscarriage, including:
- Diabetes
- Polycystic ovary syndrome (PCOS)
- Hypothyroidism
- Certain infectious diseases
- Autoimmune diseases
PCOS may increase the risk of miscarriage. Two studies suggested treatment with the drug metformin significantly lowers the rate of miscarriage in women with PCOS, but the quality of these studies has been questioned.
Infections can increase the risk of a miscarriage:
- Rubella (German measles)
- Cytomegalovirus
- Bacterial vaginosis
- HIV
- Chlamydia
- Gonorrhea
- Syphilis
- Malaria
Immune status (?????????? ?? ??????)
Autoimmunity is a possible cause of recurrent or late-term miscarriages. In the case of an autoimmune-induced miscarriage, the woman’s body attacks the growing fetus or prevents normal pregnancy progression. Autoimmune disease may cause genetic abnormalities in embryos which in turn may lead to miscarriage.
Anatomical defects and trauma (??????? ??? ?? ????)
Fifteen percent of women who have experienced three or more recurring miscarriages have some anatomical defect that prevents the pregnancy from being carried for the entire term.
In some women, cervical incompetence or cervical insufficiency occurs with the inability of the cervix to stay closed during the entire pregnancy. It does not cause the first trimester miscarriages. In the second trimester, it is associated with an increased risk of miscarriage.
Smoking (????????)
Tobacco (cigarette) smokers have an increased risk of miscarriage. There is an increased risk regardless of which parent smokes, though the risk is higher when the gestational mother smokes.
Morning sickness (???? ?? ??????)
Nausea and vomiting of pregnancy are associated with a decreased risk. Several possible causes have been suggested for morning sickness but there is still no agreement.
Chemicals and occupational exposure (????? ?? ?????????? ?????)
Chemical and occupational exposures may have some effect on pregnancy outcomes. A cause and effect relationship almost can never be established. Those chemicals that are implicated in increasing the risk for miscarriage are:
- DDT
- Lead
- Formaldehyde
- Arsenic
- Benzene
- Ethylene oxide
Video display terminals and ultrasound have not been found to have an effect on the rates of miscarriage.
In dental offices where nitrous oxide is used with the absence of anesthetic gas scavenging equipment, there is a greater risk of miscarriage. No increased risk for cosmetologists has been found.
Other risks (???? ?????)
Alcohol increases the risk of miscarriage. Progesterone has not been found to be effective in preventing miscarriage. Cocaine use increases the rate of miscarriage. Some infections have been associated with miscarriage. These include:
- Ureaplasma urealyticum
- Mycoplasma hominis
- Group B streptococci
- HIV-1
- Syphilis
Infections of Chlamydia trachomatis, Campylobacter fetus, and Toxoplasma gondii have not been found to be linked to miscarriage.

Diagnosis (?????)
In the case of blood loss, pain, or both, a transvaginal ultrasound is performed. If a viable intrauterine pregnancy is not found with ultrasound, blood tests can be performed to rule out ectopic pregnancy, which is a life-threatening situation.
If hypotension, tachycardia, and anemia are discovered, the exclusion of an ectopic pregnancy is important.
A miscarriage may be confirmed by an obstetric ultrasound and by the examination of the passed tissue.
Prevention (??????)
Prevention of a miscarriage can sometimes be accomplished by decreasing risk factors. This may include:
- Good prenatal care
- Avoiding drugs and alcohol
- Preventing infectious diseases
- Avoiding x-rays
Identifying the cause of the miscarriage may help prevent future pregnancy loss, especially in cases of recurrent miscarriage. Often there is little a person can do to prevent a miscarriage.
Vitamin supplementation before or during pregnancy has not been found to affect the risk of miscarriage.
Non-modifiable risk factors (???-?????????? ????? ?? ???)
Preventing a miscarriage in subsequent pregnancies may be enhanced with assessments of:
- Immune status
- Chemical and occupational exposures
- Anatomical defects
- Intercurrent diseases
- Previous exposure to Chemotherapy and Radiation
- Medications
- Surgical history
- Endocrine disorders
- Genetic abnormalities
Modifiable risk factors (?????????? ????? ?? ???)
Maintaining a healthy weight and good prenatal care can reduce the risk of miscarriage. Some risk factors can be minimized by avoiding the following:
- Smoking
- Cocaine use
- Alcohol
- Poor nutrition
- Occupational exposure to agents that can cause miscarriage
- Medications associated with miscarriage
- Drug abuse
Management (???????)
Women who miscarry early in their pregnancy usually do not require any subsequent medical treatment but they can benefit from support and counseling.
Most early miscarriages will complete on their own; in other cases, medication treatment or aspiration of the products of conception can be used to remove the remaining tissue.
While bed rest has been advocated to prevent miscarriage, this has not been found to be of benefit.
Significant distress can often be managed by the ability of the clinician to clearly explain terms without suggesting that the woman or couple are somehow to blame.
Methods of Treatment (????? ?? ?????)
No treatment is necessary for a diagnosis of complete miscarriage (so long as ectopic pregnancy is ruled out). In cases of an incomplete miscarriage, empty sac, or missed abortion there are three treatment options:
- Watchful waiting
- Medical management
- Surgical treatment
With no treatment (watchful waiting), most miscarriages (65–80%) will pass naturally within two to six weeks. This treatment avoids the possible side effects and complications of medications and surgery, but increases the risk of mild bleeding, need for unplanned surgical treatment, and incomplete miscarriage.
Delayed and incomplete miscarriage (??????? ?? ?????? ???????)
In delayed or incomplete miscarriage, treatment depends on the amount of tissue remaining in the uterus. Treatment can include surgical removal of the tissue with vacuum aspiration or misoprostol.
Induced miscarriage (??????? ???????)
An induced abortion may be performed by a physician for women who do not want to continue the pregnancy. Self-induced abortion performed by a woman or non-medical personnel is extremely dangerous and is still a cause of maternal mortality in some countries. In some locales, it is illegal or carries a heavy social stigma.
Support (??????)
Organizations exist that provide information and counseling to help those who have had a miscarriage. Hospitals also can provide support and help memorialize the event. Those who experience unexplained miscarriage can be treated with emotional support.
Miscarriage in other animals (???? ??????? ??? ???????)
Miscarriage occurs in all animals that experience pregnancy, though in such contexts it is more commonly referred to as a “spontaneous abortion”.
There are a variety of known risk factors in non-human animals. For example, in sheep, miscarriage may be caused by crowding through doors or being chased by dogs.
In cows, spontaneous abortion may be caused by contagious diseases, such as Brucellosis or Campylobacter, but often can be controlled by vaccination.
In many species of sharks and rays, stress-induced miscarriage occurs frequently on capture.
Female mice who had spontaneous abortions showed a sharp rise in the amount of time spent with unfamiliar males preceding the abortion than those who did not.

Miscarriage & Free Siddha Energy Remedies (??????? ?? ??:????? ????? ????? ?????)
Siddha energy remedies to be applied from day one of the pregnancy confirmed. The following suggested and tested remedies by applied as a regular activity. If a woman is trained person in Swami Hardas Life System, she knows everything about what is called UAM and should apply regularly over the stomach, which would help deliver a healthy baby naturally as well as avoid complications and miscarriage also. However, those, who are not trained should apply the remedies which include:
1. Siddha preventive measures (????? ?????? ????)
Everybody must practice Siddha preventive measures, whether a woman is having a miscarriage or not, but preventive measures are the primary steps for switching on to any other Siddha energy remedies, and hence they are important. It helps in one’s capability, effectiveness, and productivity, decision making power, intellectuality and removing minor health problems. There are three types of preventive measures:
- Earthing – performed for earthing the negativity of our body
- Field Cleaning – cleans energy field (Aura) of our body
- Siddha Brain Exercise/Energizing – energizes our brain for proper functionality
Everybody’s tendency is to get attracted toward the word ‘free‘, however, don’t neglect even these Siddha preventive measures are free. Avail the benefits by practicing them sincerely, and regularly. For the ease of understanding Siddha preventive measures, please watch a video for a live demonstration.
2. Siddha Shaktidata Yog (????? ????????? ???)
This unique Siddha Shaktidata Yog of Siddha Spirituality can solve the problems related to miscarriage with free Siddha energy remedies. There is no compulsion of training of ‘Swami Hardas Life System’ methods. This not only gives benefits to self but also it can be used for other affected persons, whether a person is in the same house, distantly available in the same city, same nation or maybe in any corner of the world, however, both the procedures have been explained here.
3. Siddha Kalyan Sadhana (????? ?????? ?????)
Recite this Sadhana with a Sankalp “My problems of miscarriage are solved as early as possible and I should gain health”, which should be repeated in mind 3 – 3 times every after each stanza. Any person irrespective of caste, creed, religion, faith, sex, and age can recite this Sadhana for free, which should be repeated at least twice in a day. To know more, please click on this link.
4. CCPE products (CCPE ??????)
These products work on the concepts of ‘Conceptual Creative Positive Energy’ (CCPE) within the provisions of ‘CCPE Life System’ and the theory of Quantum Technology to a certain extent. However, the products get activated only whenever touched by a human and then they become capable of solving the problem and achieving health. However, please use these products for miscarriage as mentioned below:
CCPE Extractor: The CCPE Extractor should be gently moved over the Agya Chakra in a circular motion at least for 30 to 60 seconds, thereafter, follow the same process on the head, and naval for another 30 to 60 seconds, which will convert negativity into positivity. This is how the process finishes within almost 2 – 3 minutes.
CCPE Booster: Keep one Booster over the Agya Chakra and another one each over the head, and naval for 3 – 5 minutes. You may need to have 3 Boosters and the process would finish within almost 2 – 3 minutes, which establishes positivity. This is how the process finishes within almost 3 minutes.
CCPE Booster powder: Add a pinch of CCPE Booster powder in a bucket of warm water. Take bath regularly in the morning for the relief from the problems/complications regarding miscarriage.
Conclusion (????????)
In view of the above, I am confident that you have learned about miscarriage, symptoms, causes, diagnosis, management, miscarriage complications, medications, and also learned free Siddha energy remedies. Now, you have become self-sufficient. Hence its right time to use your acquired knowledge for solving miscarriage related problems as per the provision available in Siddha Spirituality of Swami Hardas Life System.
However, keep learning and practicing the free Siddha Energy Remedies, which would help guide how to solve various problems regarding health, peace, and progress, without money and medicines.
DISCLAIMER
The opinions expressed in this article are the personal opinions of the concerned site owners. Siddha Spirituality For Health is not responsible for the accuracy, completeness, suitability, or validity of any information on this article. However, it is advisable to consult a specialist in the concerned field before availing the benefits. Hence we do not assume any responsibility or liability for the same.
Reference: https://en.wikipedia.org/wiki/Miscarriage

Good post.
The Ladbrokes Casino for iPhone is no less entertaining. The iOS Ladbrokes Casino app is optimized for iPhone, iPad, and iPod Touch. The full list of Playtech’s DC-branded mobile slots are available, including Batman & Catwoman Cash (and 6 other Batman slots), Superman: The Movie, and the Man of Steel Progressive Slot. Everything is mobile-compatible for Android or iPhone, along with a variety of mobile blackjack and roulette games. You can email the site owner to let them know you were blocked. Please include what you were doing when this page came up and the Cloudflare Ray ID found at the bottom of this page. Ladbrokes Poker app – 188 MBs Ladbrokes values its customers and every player who install the app and deposit funds is eligible for receiving a generous welcome bonus. The amount of your first deposit bonus is determined by the sum you top up your account with. Ladbrokes grants a 200% match bonus that cannot exceed £1,200. However, you have to meet certain wagering requirements. Your first deposit should be at least £10 and you will be given a 3-month period for clearing the full amount. Every time you get 240 Status points, £5 will be added to your bankroll. Apart from the first deposit bonus, you can also take advantage of the VIP program that guarantees a monthly rakeback of up to 35%.
http://users.atw.hu/nlw/profile.php?mode=viewprofile&u=18633
You are using an outdated browser. Please upgrade your browser to improve your experience. Cynthia R. won $24,000 when she hit a slot jackpot at Casino Arizona. The Triple Stars slot comes equipped with a paytable that includes eight standard symbols. Four of these symbols will deliver prizes that have the same value. Namely, whenever a player lands three oranges, cherries, dollar signs, or plums on a single payline, they will receive 2 times their total bet. Next on the payout table, we have the bells and watermelons. Land three matching symbols like this on a payline and you will receive 16 times the total bet. HIGH LIMIT JACKPOT ON TRIPLE STARS ★ Video Slots Online ★ HIGH LIMIT HANDPAYS! ★ Video Slots Online ★ TRIPLE DOUBLE STARS ★ Video Slots Online ★ HAPPY 4th OF JULY • The Slot Museum – Slot Machine Videos • HIGH LIMIT JACKPOT ON TRIPLE STARS • HIGH LIMIT HA
Spartan Slots Casino has a very remarkable wealth of casino games at its disposal with hundreds to choose from. Players can take their pick at all the classic table games with roulette, blackjack, and baccarat, as well as video poker and craps (including many others). This site truly excels via its slots offering, as players can enjoy games from the most popular software providers in the industry. These games range from 3 reel classics to interactive slots with fantastic bonus round features and more. Players who sign up at Spartan Slots will receive 25 free spins when they make their first deposit. This bonus is valid for both desktop and mobile users. Up until 2018, Spartan Slots casino was operating under Curacao gaming licence, however, the site seems to be running without a dedicated regulatory body at the moment. Do not bother trying to get to the bottom of the issue with the casino support team. Although reasonably kind and professional, the representatives will fail to provide precise information regarding the licence. Instead, they will generically respond that the casino is licenced by the gaming boards within the territories they operate, which is the identical line used by the client service agents in Slotastic and Jackpot Capital online casinos, suggesting two things:
https://www.homestudiolive.net/forum/general-discussions/agile-poker-cards
Pick up a generous 11 Free Spins on the Pink Elephants 2 slot with no wagering required when you deposit as little as £10 at Mr Vegas Casino. Pack your bags and head off to Vegas with Mr Vegas, an online casino with a library of over 3,000 games…. Slotguard no deposit bonus codes; topps gypsy queen hobby box; 30 ft caravan for sale australia.. May 25, 2022 · Cash Bandits Slot, ECFJ7, No Deposit Bonus, RTG. $20 + 10 FS No Deposit for Ruby Slots Casino. Code: ECFJ7. $20 + 10 FS No Deposit Bonus for all avid gamers. Playthrough: 30xB. Max Money-Out: $100. Expires on 2022-05-31. Legitimate for: Money Bandits Slot. No a number of consecutive unfastened bonuses are allowed. Love ruby slots. By far the online casino that can be played on your mobile device Gift Card Corner – Casino Bonus Library
We’ve compared some of the most lucrative online casino bonus offers available to players around the world, but be sure to check out our U.S. online casino bonus and Canada online casino bonus guides for more in-depth analysis of these regions. Playing mobile casino games these days is very easy – as most of the top-rated casinos online that offer real money games have an app or a mobile-friendly casino website. When working my way around the best online casinos, I pay attention to a number of important areas before providing you with an honest overview of my encounter. These reviews save you the time and effort of roaming aimlessly through casino deposit methods, terms and conditions, and the casino lobby. Instead, you can check out my casino comparisons, select an online casino that appeals, and make note of whether or not they tick all of your boxes.
https://www.fdb.cz/clen/207430-mostplaybetonli.html
Roll the dice on a chance to win big with our exciting, new gaming promos! Cash, cars, and more prizes! You will love the fun themes and multiple ways to become Royalty! Grab a cold one while you watch the games at Seneca Buffalo Creek Casino! Casino Credit Backlash is full-throttle metal music that pumps up the crowd and brings down the house. Get ready for one awesome show! 500 NATIONSFREE CASINO GAMESNo Signup – No Deposit As a My WinStar member, you can customize your promotion feed so you never miss a beat on whatever matters most to you. Sign up today – it’s fast, easy and free! Looking to escape the busy downtown scene of CDA? At Coeur d’Alene Casino Resort Hotel, we offer the best restaurants near Coeur d’Alene, ID. A mere 25 miles away from CDA’s downtown, you’ll admire the scenic hills of the Palouse and continue your exploration of Northern Idaho’s Panhandle. When you finish eating at one of our premier casino restaurants, win big in our 60,000-square-foot casino, rest easy in our hotel, relax at the spa, book a round of golf and attend an event you’ll love.