Gestational diabetes (???????? ??????) is a condition in which a woman without diabetes develops high blood sugar levels during pregnancy. Gestational diabetes increases the risk of pre-eclampsia, depression, and requiring a Caesarean section. Babies born to mothers are at increased risk of being too large, having low blood sugar after birth, and jaundice. Long term, children are at higher risk of being overweight and developing type 2 diabetes. There are numerous complications, hence Siddha Spirituality of Swami Hardas Life System appeal our readers to read the article and if feasible, try to undergo training of Swami Hardas Life System for better handling gestational diabetes without money and medicines.
Gestational diabetes Definition (???????? ?????? ?? ???????)
Gestational diabetes is a type of diabetes that develops during pregnancy. Diabetes means your blood glucose, also called high blood sugar. Too much glucose in your blood is not good for you or your baby. Gestational diabetes is usually diagnosed in the 24th to 28th week of pregnancy.
Managing your gestational diabetes can help you and your baby stay healthy. You can protect your own and your baby’s health by taking action right away to manage your blood glucose levels.

Gestational diabetes Classification (???????? ?????? ????????)
Gestational diabetes is formally defined as “any degree of glucose intolerance with onset or first recognition during pregnancy“. This definition acknowledges the possibility that a woman may have previously undiagnosed diabetes mellitus, or may have developed diabetes coincidentally with pregnancy.
The White classification, named after Priscilla White, who pioneered research on the effect of diabetes types on perinatal outcome, is widely used to assess maternal and fetal risk.
The two subtypes of gestational diabetes under this classification system are:
- Type A1: Abnormal oral glucose tolerance test (OGTT), but normal blood glucose levels during fasting and two hours after meals; diet modification is sufficient to control glucose levels
- Type A2: Abnormal OGTT compounded by abnormal glucose levels during fasting and/or after meals
Gestational diabetes risk factors (???????? ?????? ????? ????)
Classical risk factors for developing gestational diabetes are:
- Polycystic ovary syndrome
- A previous diagnosis of gestational diabetes or prediabetes
- A family history revealing a first-degree relative with type 2 diabetes
- Maternal age – a woman’s risk factor increases as she gets older
- Paternal age – one study found that a father’s age over 55 years was associated with gestational diabetes
- Ethnicity – those with higher risk factors include African-Americans, Afro-Caribbeans, Native Americans, Hispanics, Pacific Islanders, and people originating from South Asia
- Being overweight, obese or severely obese increases the risk
- A previous pregnancy which resulted in a child with macrosomia
- Previous poor obstetric history
- Other genetic risk factors: There are at least 10 genes where certain polymorphism are associated with an increased risk of gestational diabetes, most notably TCF7L2
In addition to this, statistics show a double risk of GDM in smokers. The polycystic ovarian syndrome (PCOS) is also a risk factor, although relevant evidence remains controversial. Some studies have looked at more controversial potential risk factors, such as short stature.

Gestational diabetes Test (???????? ?????? ???????)
To look for high levels of glucose in plasma or serum in defined circumstances, a number of screening and diagnostic tests have been used. Alternatively, a more involved diagnostic test can be used directly at the first prenatal visit for a woman with a high-risk pregnancy. (for example in those with a polycystic ovarian syndrome or acanthosis nigricans).
Non-challenge blood glucose tests (???-?????? ???? ??????? ???????)
When a plasma glucose level is found to be higher than 126 mg/dl (7.0 mmol/l) after fasting, or over 200 mg/dl (11.1 mmol/l) on any occasion, and if this is confirmed on a subsequent day, the diagnosis of GDM is made, and no further testing is required.
Screening glucose challenge test (?????????? ??????? ?????? ???????)
No previous fasting is required for this screening test, in contrast to the OGTT. The O’Sullivan test involves drinking a solution containing 50 grams of glucose and measuring blood levels 1 hour later.
If the cut-off point is set at 140 mg/dl (7.8 mmol/l), 80% of women with GDM will be detected. If this threshold for further testing is lowered to 130 mg/dl, 90% of GDM cases will be detected, but there will also be more women who will be subjected to a consequent OGTT unnecessarily.
Oral glucose tolerance test (????? ??????? ????????? ???????)
A standardized oral glucose tolerance test (OGTT) should be done in the morning after an overnight fast of between 8 and 14 hours. During the three previous days, the subject must have an unrestricted diet and unlimited physical activity. The subject should remain seated during the test and should not smoke throughout the test.
The test involves drinking a solution containing a certain amount of glucose, usually 75 g or 100 g, and drawing blood to measure glucose levels at the start and onset time intervals thereafter.
The following are the values which the American Diabetes Association considers to be abnormal during the 100 g of glucose OGTT:
- Fasting blood glucose level ?95 mg/dl (5.33 mmol/L)
- 1-hour blood glucose level ?180 mg/dl (10 mmol/L)
- 2-hour blood glucose level ?155 mg/dl (8.6 mmol/L)
- 3-hour blood glucose level ?140 mg/dl (7.8 mmol/L)
Urinary glucose testing (????? ??? ??????? ???????)
Women with GDM may have high glucose levels in their urine. However, urinary glucose testing may be undertaken.
Gestational diabetes Prevention (???????? ?????? ?? ??????)
It has been suggested that for women who have had gestational diabetes, support between pregnancies may lower their chances of having gestational diabetes again in future pregnancies. This support might include diet and exercise, education, and lifestyle advice.
However, there is no research to show whether interventions between pregnancies lower the number of women who develop gestational diabetes again. Theoretically, smoking cessation may decrease the risk of gestational diabetes among smokers.
Gestational Diabetes Management (???????? ?????? ?? ???????)
Lifestyle interventions include:
- Exercise
- Diet advice
- Behavioral interventions
- Relaxation
- Self-monitoring glucose
- Combined interventions
Women with gestational diabetes who receive lifestyle interventions seem to have less postpartum depression and were more likely to reach their weight loss targets after giving birth, than women who had no intervention. Their babies are also less likely to be large for their gestational age and have less percentage of fat when they are born. More research is needed to find out which lifestyle interventions are best.
Gestational diabetes Lifestyle (???????? ?????? ???? ????)
Counseling before pregnancy and multidisciplinary management are important for good pregnancy outcomes. Most women can manage their GDM with dietary changes and exercise. Self-monitoring of blood glucose levels can guide therapy. Some women will need antidiabetic drugs, most commonly insulin therapy.
Diet (????)
Since insulin resistance is highest in mornings, breakfast carbohydrates need to be restricted more. Ingesting more fiber in foods with whole grains, or fruit and vegetables can also reduce the risk of gestational diabetes. There is not enough evidence to indicate if one type of dietary advice is better than another.
Exercise (???????)
Regular moderately intense physical exercise is advised, although there is no consensus on the specific structure of exercise programs for GDM. Pregnant women who exercise have lower blood sugar levels when fasting and after meals compared to those who do not exercise. It is not clear which form of exercise is best when pregnant.
Self-monitoring (????? ???????)
Compliance with these glucometer systems can be lower. Self-monitoring can be accomplished using a handheld capillary glucose dosage system. Target ranges advised by the Australasian Diabetes in Pregnancy Society are as follows:
- Fasting capillary blood glucose levels <5.5 mmol/L
- 1-hour postprandial capillary blood glucose levels <8.0 mmol/L
- 2-hour postprandial blood glucose levels <6.7 mmol/L
Regular blood samples can be used to determine HbA1c levels, which give an idea of glucose control over a longer time period. Research suggests a possible benefit of breastfeeding to reduce the risk of diabetes and related risks for both mother and child.
Gestational diabetes Medication (???????? ?????? ???)
If monitoring reveals failing control of glucose levels with these measures, or if there is evidence of complications like excessive fetal growth, treatment with insulin might be necessary.
Care needs to be taken to avoid low blood sugar levels due to excessive insulin. Insulin therapy can be normal or very tight; more injections can result in better control but require more effort, and there is no consensus that it has large benefits.
Another review found good short term safety for both the mother and baby with metformin but unclear long term safety. People may prefer metformin by mouth to insulin injections. Treatment of polycystic ovarian syndrome with metformin during pregnancy has been noted to decrease GDM levels.
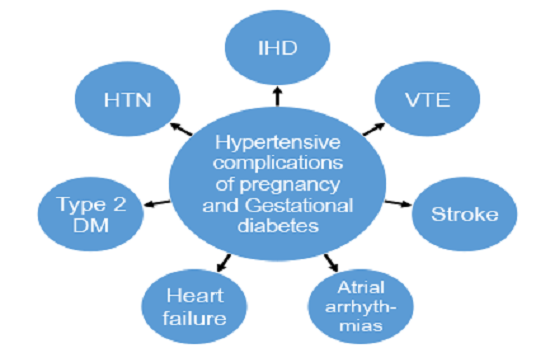
Gestational diabetes Complications (???????? ?????? ?? ????????)
GDM poses a risk to mother and child. This risk is largely related to uncontrolled blood glucose levels and its consequences. The risk increases with higher blood glucose levels. Treatment resulting in better control of these levels can reduce some of the risks of GDM considerably.
Neonates born from women with consistently high blood sugar levels are also at an increased risk of:
- Low blood glucose (hypoglycemia)
- Jaundice
- High red blood cell mass (polycythemia)
- Low blood calcium (hypocalcemia) and magnesium (hypomagnesemia)
Untreated GDM also interferes with maturation, causing dysmature babies prone to respiratory distress syndrome due to incomplete lung maturation and impaired surfactant synthesis.
Gestational diabetes & Free Siddha Energy Remedies (???????? ?????? ?? ??:????? ????? ????? ?????)
As there are no treatments to cure any type of diabetes, one may resort to other sources e.g. Ayurveda, Homeopathy, Yoga, Home remedies, which depends on the choice of the sufferer. One may also try the free Siddha energy remedies mentioned in the article named diabetes mellitus. Desirous persons can undergo training of Swami Hardas Life System, just learn the methods and apply instantly. The benefits are sure.
In addition to the Siddha energy remedies suggested in the article – Diabetes Mellitus & Free Siddha Energy Remedies, also perform Swayamsiddha Agnihotra mentioned in the article – Air Pollution & Swayamsiddha Agnihotra.
Training of Swami Hardas Life System (?????? ????? ???? ?????? ?? ?????????)
Any problem with regard to health, peace, and progress can be solved independently without money and medicines by undergoing training of Swami Hardas Life System. Any person irrespective of religion, caste, creed, faith, sex, and age can undergo this unique training.
Conclusion (????????)
In view of the above, I am confident that you have learned about Gestational diabetes, definition, classification, risk factors, prevention, management, complications, gestational diabetes test, medication, and also learned free Siddha energy remedies. Now, you have become self-sufficient. Hence its right time to use your acquired knowledge for solving problems as per the provision available in Siddha Spirituality of Swami Hardas Life System.
However, keep learning and practicing the free Siddha Energy Remedies, which would help guide how to solve various problems regarding health, peace, and progress, without money and medicines.
DISCLAIMER
The opinions expressed in this article are the personal opinions of the concerned site owners. Siddha Spirituality For Health is not responsible for the accuracy, completeness, suitability, or validity of any information on this article. However, it is advisable to consult a specialist in the concerned field before availing the benefits. Hence we do not assume any responsibility or liability for the same.
Reference: https://en.wikipedia.org/wiki/Gestational_diabetes

Meaningful Article.Thanks for sharing.
Nice post.
Nice post
Быстрая схема покупки диплома старого образца: что важно знать?
odnopolchane.net/forum/member.php?u=546804