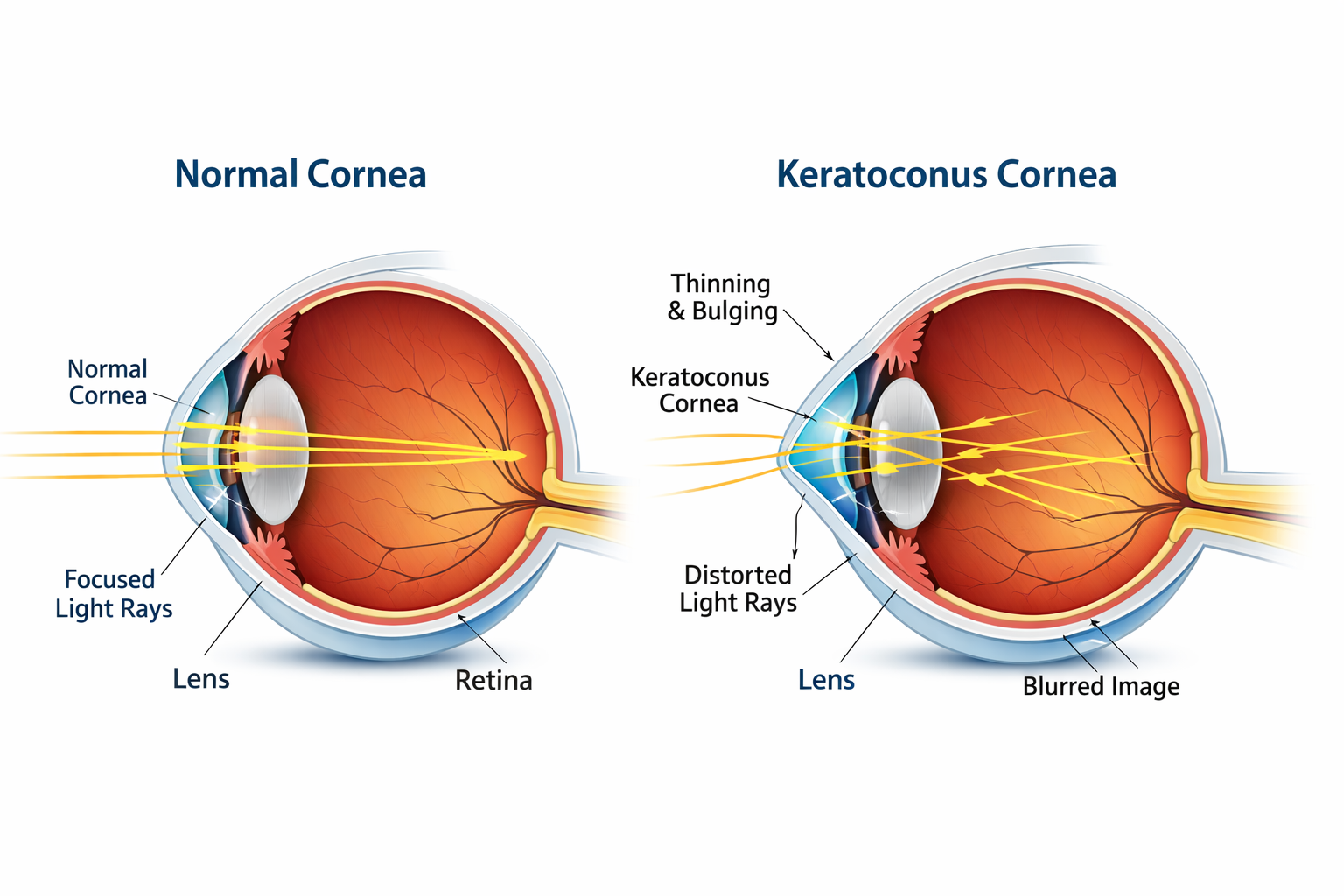
Keratoconus (कॉर्निया शंकु) is an eye disorder in which the cornea, the transparent front part of the eye, gradually thins and bulges outward into a cone shape. This causes distorted vision, including blurry vision, double vision, increased nearsightedness, irregular astigmatism, and light sensitivity, which can reduce quality of life. Both eyes are usually affected.
Keratoconus affects about 1 in 2,000 people, though some estimates suggest it may be as common as 1 in 400. It typically develops in late childhood or early adulthood and occurs in all populations, though it may be more common in some ethnic groups, such as people of Asian descent. The name comes from the Greek kéras (cornea) and Latin cōnus (cone).
What Is Keratoconus?
Keratoconus is an eye condition in which the cornea, the clear dome-shaped surface at the front of the eye, gradually becomes thinner and bulges outward into a cone-like shape. Normally, the cornea is round and smooth, allowing light to focus properly on the retina. When it becomes irregular, light scatters, distorting vision.
The condition usually affects both eyes, though one eye may worsen faster than the other. Keratoconus often begins during the teenage years or early adulthood and may progress for 10–20 years before stabilizing.
According to the National Eye Institute, early diagnosis plays a crucial role in slowing progression and preserving visual clarity.
Why Keratoconus Matters?
Keratoconus is not just about needing stronger glasses. As the cornea changes shape, everyday activities such as reading, driving at night, using digital screens, and recognizing faces can become challenging.
If left untreated, advanced keratoconus may lead to:
-
Severe visual distortion
-
Frequent prescription changes
-
Contact lens intolerance
-
Corneal scarring
-
Significant reduction in quality of life
However, the encouraging news is that modern ophthalmology offers highly effective treatment options.
Symptoms of Keratoconus
Symptoms often appear gradually, which is why many people mistake early keratoconus for simple refractive errors.
Early Symptoms
-
Mild blurring of vision
-
Increased sensitivity to light
-
Frequent changes in eyeglass prescription
-
Difficulty seeing clearly at night
-
Eye strain and headaches
Progressive Symptoms
As the cornea continues to thin and bulge:
-
Distorted or wavy vision
-
Double vision in one eye
-
Increased nearsightedness
-
Irregular astigmatism
-
Halos around lights
-
Glare while driving
Advanced Symptoms
In severe stages:
-
Sudden worsening of vision
-
Corneal scarring
-
Extreme light sensitivity
-
Poor correction, even with glasses
The American Academy of Ophthalmology emphasizes that rapidly changing prescriptions — especially in teenagers — should never be ignored.
What Causes Keratoconus?
The exact cause is not fully understood, but researchers believe it results from a combination of genetic, environmental, and biochemical factors.
Genetic Predisposition
If a close family member has keratoconus, the risk increases significantly.
Weak Corneal Structure
The cornea is made primarily of collagen fibers. When these fibers weaken, the cornea loses its ability to maintain shape.
Chronic Eye Rubbing
One of the most strongly associated risk factors. Persistent rubbing may damage corneal tissue over time.
Oxidative Stress
An imbalance between harmful free radicals and protective antioxidants can weaken corneal cells.
Associated Conditions
Keratoconus is sometimes linked with:
-
Severe allergies
-
Connective tissue disorders
Health organizations such as the World Health Organization highlight the importance of routine eye examinations for early detection of progressive eye diseases.
Who Is Most at Risk?
Anyone can develop keratoconus, but certain factors increase susceptibility:
-
Onset during adolescence
-
Family history
-
Habitual eye rubbing
-
Chronic allergic eye disease
-
Poorly managed atopic conditions
The disorder affects people worldwide and is increasingly detected due to improved diagnostic technologies.
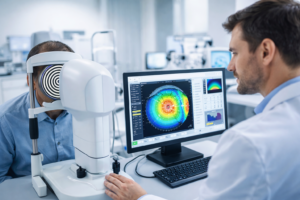
How is Keratoconus Diagnosed?
Early diagnosis is critical because modern treatments can halt progression but cannot fully reverse structural changes.
An eye specialist may perform the following tests:
Corneal Topography
Creates a detailed map of the cornea’s curvature and is considered the gold standard for detecting keratoconus.
Pachymetry
Measures corneal thickness to identify abnormal thinning.
Refraction Test
Determines how light bends in the eye and reveals irregular astigmatism.
Slit-Lamp Examination
Allows the doctor to examine the cornea under magnification.
Routine eye exams are especially important for young individuals experiencing rapid changes in vision.
Stages of Keratoconus
Understanding the stages helps guide treatment decisions.
Mild Stage
-
Slight corneal steepening
-
Glasses usually provide adequate correction
Moderate Stage
-
Increasing irregular astigmatism
-
Soft lenses may no longer help
-
Specialized contact lenses are often required
Advanced Stage
-
Significant corneal thinning
-
Vision severely distorted
-
Surgical options may be necessary
Treatment Options for Keratoconus
Treatment depends largely on the severity and progression of the disease.
Eyeglasses or Soft Contact Lenses
Effective only in the earliest stages when the cornea remains relatively regular.
Rigid Gas Permeable (RGP) Lenses
These lenses create a smooth optical surface, dramatically improving vision.
Scleral Lenses
Larger lenses that vault over the cornea and rest on the sclera. They are often more comfortable and provide excellent visual quality.
Corneal Collagen Cross-Linking (CXL)
One of the most important breakthroughs in keratoconus management.
How does it work?
-
Riboflavin (vitamin B2) drops are applied
-
The cornea is activated with UV light
-
Collagen fibers strengthen
Goal: Stop progression — not necessarily improve vision.
When performed early, cross-linking can prevent the need for future surgery.
Intacs (Corneal Ring Segments)
Tiny arc-shaped implants are inserted into the cornea to flatten its cone shape.
Corneal Transplant
Reserved for severe cases with scarring or extreme thinning.
Success rates are generally high, and many patients regain functional vision.
Can Keratoconus Be Prevented?
There is no guaranteed prevention, but risk can be significantly reduced.
Avoid Eye Rubbing
This is one of the most actionable protective steps.
Manage Allergies
Treat itchy eyes promptly to reduce rubbing.
Schedule Regular Eye Exams
Especially important for teenagers and young adults.
Protect Your Eyes
Use UV-protective sunglasses when outdoors.
Maintain Nutritional Health
Antioxidant-rich foods may support cellular health.
Ayurveda Treatment for Keratoconus
In Ayurveda, eye health is closely linked to the balance of the body’s three doshas — Vata, Pitta, and Kapha. Keratoconus is often interpreted as a condition involving weakened ocular tissues and aggravated Vata, sometimes combined with excess Pitta that may contribute to inflammation or sensitivity. While Ayurveda does not reverse the structural cone shape, it aims to strengthen eye tissues, improve nourishment, and slow functional deterioration.
Common Ayurvedic Approaches
Netra Tarpana (Eye Nourishment Therapy)
A deeply rejuvenating treatment in which medicated ghee is retained around the eyes inside a dough ring. It is believed to lubricate ocular tissues, reduce dryness, and support corneal health.
Triphala Eye Wash
A gentle herbal decoction traditionally used to cleanse the eyes. Triphala is valued for its antioxidant properties that may help protect delicate eye structures.
Herbal Ghee Preparations
Medicated ghritas are sometimes recommended to promote tissue regeneration and improve visual clarity by enhancing internal lubrication.
Nasya Therapy
Application of herbal oils through the nasal passages is thought to support head and sensory organ health, including the eyes.
Diet and Lifestyle Guidance
Ayurveda emphasizes prevention through:
-
Antioxidant-rich foods
-
Adequate hydration
-
Reduced screen strain
-
Avoiding excessive eye rubbing
-
Proper sleep
Important: Ayurvedic care should be considered supportive, not a replacement for medical treatments such as corneal cross-linking or specialty lenses. Always consult a qualified eye specialist before beginning alternative therapies.

Best Home Remedies for Keratoconus
Avoid Eye Rubbing (Most Important)
Repeated eye rubbing is strongly linked to faster corneal thinning.
What to do?
-
If your eyes itch, use preservative-free lubricating drops.
-
Treat allergies promptly.
-
Keep your hands clean and away from your eyes.
This single habit change can significantly protect corneal stability.
Use Lubricating Eye Drops
Dryness increases irritation and the urge to rub your eyes.
Benefits
-
Keeps the ocular surface hydrated
-
Improves comfort for contact lens users
-
Reduces micro-trauma from friction
Choose artificial tears recommended by your eye specialist.
Increase Antioxidant Intake
Oxidative stress is believed to weaken corneal tissue.
Eat more
-
Leafy greens (spinach, kale)
-
Citrus fruits
-
Carrots
-
Nuts and seeds
-
Berries
Nutrients like Vitamin C, Vitamin E, and omega-3 fatty acids support cellular health.
Wear UV-Protective Sunglasses
Ultraviolet exposure may contribute to tissue damage over time.
Look for
-
99–100% UVA/UVB protection
-
Wraparound frames for better coverage
Make sunglasses a daily habit — not just a summer accessory.
Manage Screen Time
Digital strain does not cause keratoconus, but it can worsen discomfort.
Follow the 20-20-20 rule: Every 20 minutes, look at something 20 feet away for 20 seconds.
Also, remember to blink frequently to prevent dryness.
Prioritize Quality Sleep
Your eyes repair themselves during sleep.
Lack of rest can lead to:
-
Eye fatigue
-
Increased sensitivity
-
Blurred vision
Aim for 7–8 hours nightly.
Control Allergies
Chronic allergies often trigger aggressive eye rubbing.
Helpful steps
-
Keep windows closed during high pollen days
-
Use air purifiers
-
Wash your face after outdoor exposure
Consult a doctor if symptoms persist.
Maintain Proper Contact Lens Hygiene
If you wear specialty lenses:
-
Clean them exactly as directed
-
Never sleep in lenses unless approved
-
Replace them on schedule
Poor hygiene raises infection risk, which can further damage the cornea.
Stay Hydrated
Dehydration can worsen ocular dryness.
A simple guideline: Drink enough water so your urine remains pale yellow.
Schedule Regular Eye Exams
Early detection of progression allows timely treatments such as corneal cross-linking, widely supported by the National Eye Institute.
Even if your vision feels stable, do not skip follow-ups.
Important
Home remedies support comfort and protection, but they cannot reshape the cornea. If you notice rapidly worsening vision, glare, or frequent prescription changes, seek professional care promptly.
Expert Tip (Often Overlooked)
Stop rubbing your eyes. Eye specialists consistently identify this as the most preventable risk factor for keratoconus progression.
Living with Keratoconus
A diagnosis can feel overwhelming, but most people continue to lead active, productive lives.
Practical Tips
-
Keep prescriptions updated
-
Follow lens hygiene strictly
-
Attend follow-up appointments
-
Discuss new symptoms immediately
Mental and Emotional Well-being
Vision changes can impact confidence and independence. Seeking support from eye care professionals and patient communities can make adaptation easier.
Remember — keratoconus is manageable, especially with early intervention.
When Should You See an Eye Doctor?
Seek evaluation if you notice:
-
Rapidly worsening vision
-
Frequent prescription changes
-
Persistent glare or halos
-
Difficulty driving at night
-
Blurred vision that glasses cannot correct
Prompt care can preserve long-term eye health.
Future Advances in Keratoconus Care
Research continues to improve outcomes. Emerging areas include:
-
Customized cross-linking
-
Advanced topography-guided treatments
-
Regenerative corneal therapies
-
Improved transplant techniques
The future looks promising, with earlier detection and less invasive management becoming increasingly accessible.
Conclusion
Keratoconus is a progressive yet highly manageable eye disorder. While the thinning and cone-shaped bulging of the cornea can distort vision and interfere with daily activities, modern diagnostic tools allow doctors to identify the condition earlier than ever before.
Treatments such as specialized contact lenses and corneal collagen cross-linking have transformed patient outcomes, often preventing severe vision loss. The key lies in awareness — recognizing early symptoms, avoiding harmful habits like eye rubbing, and committing to regular eye examinations.
If you or a loved one experiences unexplained visual changes, do not delay seeking professional advice. With timely care and the right treatment plan, individuals with keratoconus can maintain clear vision and a high quality of life for years to come.
FAQs About Keratoconus
1. What is keratoconus?
Keratoconus is a progressive eye disorder in which the cornea gradually thins and bulges outward into a cone shape. This irregular curvature prevents light from focusing properly on the retina, leading to blurred and distorted vision that often worsens over time.
2. What are the early signs of keratoconus?
Early symptoms usually include mild blurring, increased sensitivity to light, and frequent changes in eyeglass prescription. Many people initially assume their eyesight is simply getting weaker, which is why regular eye exams are important for early detection.
3. What causes keratoconus?
The exact cause is not fully known, but experts believe it results from a combination of genetic predisposition, chronic eye rubbing, allergies, and weakened collagen fibers within the cornea. Environmental factors and oxidative stress may also contribute to its development.
4. At what age does keratoconus typically begin?
Keratoconus commonly starts during the teenage years or early twenties, though it can appear later in some individuals. The condition often progresses for several years before stabilizing, making early monitoring essential.
5. Can keratoconus lead to blindness?
Keratoconus rarely causes complete blindness. However, if left untreated, it can result in severe visual impairment that interferes with daily activities. Fortunately, modern treatments allow most people to maintain functional vision.
6. How is keratoconus diagnosed?
Eye specialists use advanced imaging tests such as corneal topography to map the curvature of the cornea and detect even subtle irregularities. Comprehensive eye exams help determine the severity and guide appropriate treatment.
7. Is keratoconus hereditary?
Yes, genetics can play a role. Individuals with a family history of keratoconus have a higher risk of developing the condition, which is why proactive screening is often recommended for close relatives.
8. What treatments are available for keratoconus?
Treatment depends on severity and may include eyeglasses, specialized contact lenses, or procedures designed to strengthen the cornea. One widely recommended treatment is corneal collagen cross-linking, supported by the American Academy of Ophthalmology, which can help slow or stop progression.
9. Can keratoconus be cured naturally?
There is currently no natural cure that can restore the cornea’s original shape. Healthy lifestyle habits and home care can support eye comfort, but medical supervision remains essential to prevent worsening.
10. What is the most important precaution for people with keratoconus?
Avoiding eye rubbing is considered one of the most critical preventive measures. Protecting the eyes from mechanical stress, attending regular checkups, and following professional guidance greatly improve long-term visual outcomes.
Reference: https://en.wikipedia.org/wiki/Keratoconus