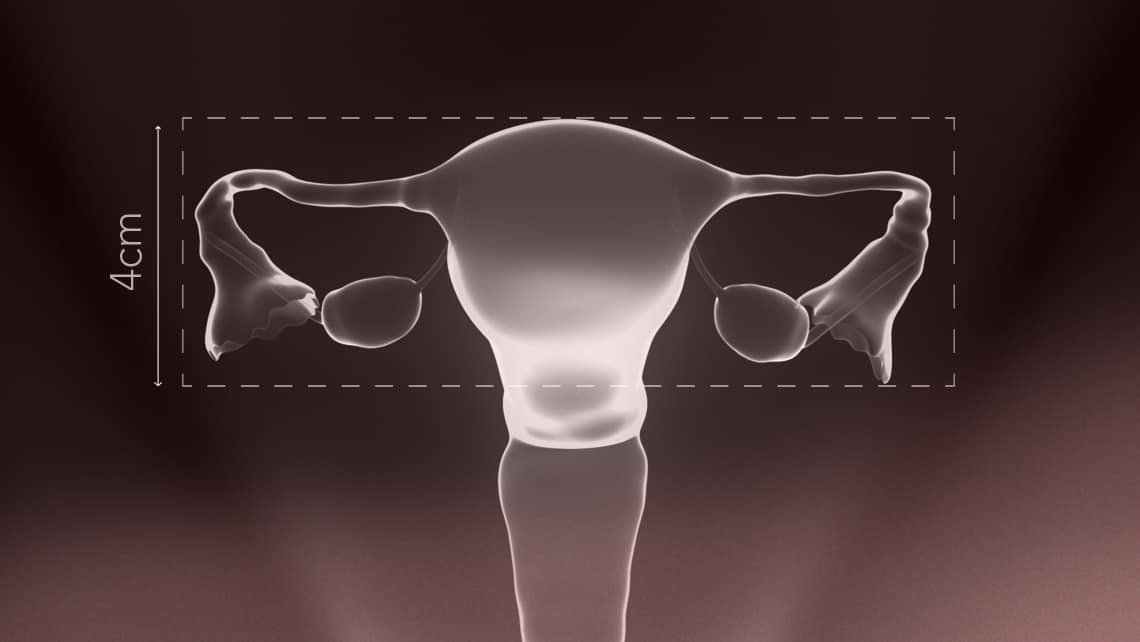
Uterine Hypoplasia (गर्भाशय हाइपोप्लेसिया) is a reproductive disorder where the uterus is smaller than expected (hypoplasia). Infantile uterus is a disorder where an adult uterus has the proportions of an immature uterus; an infantile uterus can be too small (hypoplastic), but can also be of normal size. Both conditions can be related to hypogonadism. They may be treated with hormone therapy using estrogens or with surgery to expand the uterine cavity. There is no consensus on the exact definitions of either term. One study of 29 women with uterine hypoplasia found that their uteri were cylindrical in shape. The length and shape of the uterus can be measured by ultrasound, while hysteroscopy is used to investigate the interior of the uterus. Magnetic resonance imaging (MRI) and hysterosalpingography (HSG) are also used in analyzing and diagnosing uterine hypoplasia.
What is Hypoplasia?
Hypoplasia is a medical term that refers to the underdevelopment or incomplete development of a tissue or organ due to a reduced number of cells. It differs from aplasia (complete absence of development) because in hypoplasia, the organ or tissue is present but smaller or less developed than it would be normally.
What is Uterine Hypoplasia?
Uterine hypoplasia (also called infantile uterus or underdeveloped uterus) is a condition in which the uterus is present but smaller and underdeveloped compared to the normal size for a woman’s age. It results from incomplete development of the uterus during puberty, often due to hormonal or developmental disturbances.
What are the Risk Factors for Uterine Hypoplasia?
Uterine hypoplasia develops when something interferes with the normal growth of the uterus during childhood or puberty. The risk factors are those conditions or influences that increase a girl’s likelihood of developing it.
Genetic & Chromosomal Factors
-
Turner syndrome (45, XO) – ovarian dysgenesis prevents proper uterine growth.
-
Other chromosomal abnormalities affecting the gonads or hormones.
-
Family history of reproductive developmental disorders.
Hormonal & Endocrine Factors
-
Ovarian insufficiency (reduced estrogen production).
-
Pituitary or hypothalamic dysfunction (low FSH/LH secretion).
-
Thyroid disorders (hypothyroidism, hyperthyroidism).
-
Hyperprolactinemia (high prolactin levels suppress reproductive hormones).
Nutritional & Developmental Factors
-
Childhood malnutrition or poor dietary intake.
-
Severe underweight (low body fat → low estrogen).
-
Chronic illnesses in childhood/adolescence (e.g., tuberculosis, anemia, diabetes).
Lifestyle & Environmental Factors
-
Excessive physical training (e.g., in athletes, dancers, gymnasts).
-
Exposure to environmental toxins, pesticides, and endocrine-disrupting chemicals.
Iatrogenic (Medical) Factors
-
Pelvic radiation therapy during childhood.
-
Chemotherapy affects the ovaries and reproductive organs.
-
Long-term use of hormone-suppressing medications.
Summary
Risk factors for uterine hypoplasia include:
-
Genetic syndromes (like Turner’s)
-
Hormonal imbalances (estrogen deficiency, thyroid/pituitary disorders)
-
Nutritional deficiencies and chronic illness
-
Stress, over-exercise, and low body weight
-
Medical treatments (radiation/chemotherapy in childhood)
These factors either reduce estrogen stimulation or directly impair uterine development, leading to hypoplasia.
Symptoms of Uterine Hypoplasia
Uterine hypoplasia often shows up through problems related to menstruation, puberty, and fertility. The symptoms can vary depending on how underdeveloped the uterus is and whether it is linked to hormonal or genetic issues.
Menstrual Problems
-
Primary amenorrhea – absence of the first menstrual period.
-
Oligomenorrhea – infrequent or irregular menstrual cycles.
-
Hypomenorrhea – very light menstrual flow.
-
Dysmenorrhea – painful periods (in some cases).
Delayed or Incomplete Puberty
-
Lack of normal breast development.
-
Poor development of secondary sexual characteristics (e.g., body hair, hips).
-
Underdeveloped external genitalia.
Infertility Issues
-
Difficulty conceiving due to a small uterine cavity.
-
Increased risk of miscarriage if pregnancy occurs.
Pelvic and General Symptoms
-
Pelvic pain or discomfort.
-
A small or underdeveloped uterus is found on pelvic exam or ultrasound.
-
Short stature or other physical signs are associated with genetic syndromes (e.g., Turner syndrome).
In short, the main symptoms are absent/irregular periods, delayed puberty, infertility, and sometimes pelvic pain.
Causes of Uterine Hypoplasia
Uterine hypoplasia develops when the uterus does not grow to its normal size, usually due to hormonal, genetic, nutritional, or systemic factors that interfere with development during childhood or puberty.
Hormonal Causes
-
Low estrogen levels → inadequate stimulation of uterine growth during puberty.
-
Hypothalamic or pituitary dysfunction → reduced secretion of GnRH, FSH, and LH.
-
Ovarian insufficiency (e.g., premature ovarian failure).
-
Endocrine disorders such as hypothyroidism, hyperprolactinemia, or adrenal dysfunction.
Genetic & Congenital Causes
-
Turner syndrome (45, XO) → ovarian dysgenesis leading to an underdeveloped uterus.
-
Other chromosomal abnormalities affecting gonadal function.
-
Congenital malformations of the Müllerian ducts (though these usually cause agenesis or structural anomalies rather than hypoplasia).
Nutritional & Developmental Causes
-
Malnutrition during childhood or adolescence → delays puberty and uterine growth.
-
Chronic illnesses (e.g., anemia, tuberculosis, or systemic diseases) can significantly impact overall development.
Iatrogenic Causes
-
Radiation therapy to the pelvis during childhood.
-
Chemotherapy leads to ovarian and uterine underdevelopment.
-
Long-term use of certain medications (rare).
Other Contributing Factors
-
Severe psychological stress or trauma in adolescence can delay puberty.
-
Excessive physical training or eating disorders → low body fat, leading to estrogen deficiency.
Uterine hypoplasia is usually caused by hormonal insufficiency, genetic syndromes, poor nutrition, or chronic illness that prevents normal uterine growth during puberty.
Diagnosis of Uterine Hypoplasia
Uterine hypoplasia is diagnosed by combining clinical evaluation, imaging studies, and hormonal/genetic tests to confirm that the uterus is present but underdeveloped.
Medical History & Physical Examination
-
History of absent or irregular periods (primary/secondary amenorrhea, oligomenorrhea).
-
History of delayed puberty or infertility.
-
Physical exam may reveal delayed development of secondary sexual characteristics (breasts, body hair).
-
A pelvic exam may show a small or underdeveloped uterus and cervix.
Imaging Studies
-
Pelvic Ultrasound (USG):
-
Most common first-line test.
-
Shows the uterus is smaller than normal (uterine body–cervix ratio immature).
-
Helps rule out agenesis or other Müllerian anomalies.
-
-
MRI (Magnetic Resonance Imaging):
-
Provides a more detailed view of uterine size, shape, and structure.
-
Useful in complex or unclear cases.
-
Laboratory (Hormonal) Tests
-
Estrogen, FSH, and LH levels – to check ovarian and pituitary function.
-
Thyroid function tests (TSH, T3, T4) – since hypothyroidism may contribute.
-
Prolactin levels – to rule out hyperprolactinemia.
-
Androgen levels – to assess hormonal balance.
Genetic / Chromosomal Studies
-
Karyotyping – to detect genetic syndromes (e.g., Turner syndrome 45, XO).
-
Molecular testing – in selected cases, if suspected chromosomal microdeletions or abnormalities.
Other Tests
-
Bone age assessment (X-ray of wrist/hand) – to check delayed puberty.
-
Endocrine evaluation – if pituitary or hypothalamic dysfunction is suspected.
Uterine hypoplasia is diagnosed by pelvic imaging (ultrasound/MRI) supported by hormonal testing, genetic analysis, and clinical evaluation of puberty and menstrual history.

Preventive Measures for Uterine Hypoplasia
Since uterine hypoplasia usually develops due to genetic, hormonal, nutritional, or systemic issues during growth, prevention mainly focuses on promoting healthy development in childhood and adolescence and early management of risk factors.
Nutrition & Lifestyle
-
Ensure a balanced diet rich in proteins, vitamins (A, D, E, K), iron, and minerals for proper growth.
-
Prevent malnutrition and severe underweight in girls.
-
Encourage regular physical activity but avoid overtraining (common in athletes, dancers, gymnasts), as excessive exercise with low body fat can suppress estrogen production.
-
Maintain a healthy body weight (both underweight and extreme obesity may disturb hormones).
Hormonal & Reproductive Health
-
Early detection and treatment of delayed puberty.
-
Regular check-ups for menstrual irregularities in teenage girls.
-
Timely treatment of endocrine disorders (thyroid problems, pituitary/hypothalamic issues, PCOS, adrenal dysfunction).
-
Avoid unnecessary or prolonged use of medications that can affect hormones.
General Health Measures
-
Prevent and treat chronic illnesses (anemia, tuberculosis, systemic infections) during childhood.
-
Manage psychological stress and provide emotional support, since severe stress during puberty can delay sexual development.
-
Encourage adequate sleep and healthy daily routines.
Medical Monitoring
-
Pediatric and adolescent gynecology check-ups for girls with growth delays.
-
Ultrasound scans if delayed puberty or amenorrhea is suspected, so that underdevelopment can be detected early.
-
Genetic counseling for families with known chromosomal conditions (like Turner syndrome).
Iatrogenic / Environmental Prevention
-
Minimize exposure of young girls to pelvic radiation or chemotherapy, unless necessary.
-
Protect children from environmental toxins, endocrine disruptors, and smoking exposure, which may affect reproductive health.
Uterine hypoplasia can often be prevented or minimized by good nutrition, early detection of hormonal or genetic problems, timely treatment of menstrual disorders, and protecting overall health during childhood and puberty.
Best Treatments for Uterine Hypoplasia
Since uterine hypoplasia means the uterus is present but underdeveloped, the goal of treatment is to stimulate uterine growth, correct hormonal imbalances, and restore menstrual/reproductive function as much as possible.
Hormone Replacement Therapy (HRT)
-
Estrogen therapy → stimulates growth of the uterus, endometrium, and secondary sexual characteristics (breasts, hips).
-
Cyclic estrogen + progesterone → helps mimic natural menstrual cycles and prepare the uterus for possible pregnancy.
-
Usually starts during adolescence if hypoplasia is diagnosed early.
Treatment of Underlying Causes
-
Ovarian insufficiency / gonadal dysgenesis → HRT is lifelong in many cases.
-
Thyroid or pituitary disorders → corrected with appropriate medications (thyroxine, dopamine agonists, gonadotropins, etc.).
-
Nutritional deficiencies → proper diet, vitamins, and supplementation.
-
Chronic illnesses → treated to restore overall growth.
Fertility Treatments
-
If natural conception is difficult:
-
Ovulation induction medications (if ovaries are functional).
-
Assisted Reproductive Technologies (ART):
-
In vitro fertilization (IVF) – in selected cases with partial uterine development.
-
IVF with gestational surrogacy – if the uterine cavity is too small or non-functional to carry a pregnancy.
-
-
Adjunctive & Supportive Therapies
-
Physical therapy / pelvic massage (in some traditions like Ayurveda & Unani) – claimed to improve pelvic circulation (limited scientific evidence).
-
Psychological counseling – for emotional support, especially if infertility is present.
-
Healthy lifestyle – balanced diet, avoiding over-exercise, and stress management to support hormonal balance.
Surgical Interventions
-
Rarely used, but in some cases of associated uterine malformations, surgery may be considered.
-
For isolated hypoplasia, surgery usually has a limited role.
Summary
The best treatment depends on the cause and severity:
-
Mild cases → Hormone therapy can stimulate uterine growth and restore menstruation/fertility.
-
Moderate cases → HRT + fertility support may be required.
-
Severe cases → Uterus may remain too small, and IVF with surrogacy is often the best option.
Home Remedies for Uterine Hypoplasia
Since uterine hypoplasia is primarily due to hormonal or developmental causes, there are no home remedies that can “cure” it completely. Medical treatments (especially hormone therapy) are essential in most cases. However, certain home-based and lifestyle measures can support uterine and hormonal health, improve the effectiveness of medical therapy, and promote overall reproductive well-being.
Balanced Nutrition
-
Eat foods that naturally support hormone production:
-
Healthy fats (avocado, nuts, seeds, olive oil, ghee).
-
Protein-rich foods (lentils, beans, eggs, fish, dairy).
-
Iron & folate sources (green leafy vegetables, beetroot, dates).
-
Zinc & selenium sources (pumpkin seeds, sesame seeds, sunflower seeds, whole grains).
-
-
Avoid junk food, excess caffeine, and refined sugar, as these can disrupt hormone balance.
Herbal & Natural Remedies (supportive, not curative)
(These should be taken with medical advice to avoid interactions)
-
Ashwagandha – balances stress hormones, supports reproductive health.
-
Shatavari (Asparagus racemosus) – traditionally used in Ayurveda for female reproductive development.
-
Flaxseeds – rich in phytoestrogens that gently support estrogen balance.
-
Ginger & turmeric – improve blood circulation and reduce inflammation.
Lifestyle Practices
-
Maintain a healthy weight – both underweight and obesity can worsen hormonal imbalance.
-
Moderate exercise – yoga, walking, cycling → improves pelvic blood circulation.
-
Avoid over-exercising – extreme workouts can lower estrogen levels and worsen hypoplasia.
-
Stress management – meditation, pranayama (breathing exercises), journaling, or mindfulness reduces cortisol (stress hormone), which otherwise interferes with estrogen.
Yoga & Pelvic Exercises
Certain yoga poses may improve blood flow to the pelvic region:
-
Bhujangasana (Cobra pose)
-
Setu Bandhasana (Bridge pose)
-
Baddha Konasana (Butterfly pose)
-
Paschimottanasana (Seated forward bend)
General Care
-
Ensure adequate sleep (7–8 hours daily) for hormonal regulation.
-
Avoid exposure to endocrine disruptors (plastics, pesticides, cosmetics with parabens).
-
Stay hydrated and maintain a regular daily routine.
Home remedies cannot replace medical treatment (like hormone replacement therapy) for uterine hypoplasia. They are best used as complementary measures to support reproductive health, improve overall vitality, and enhance the effectiveness of medical management.

Ayurveda Treatments for Uterine Hypoplasia
Let me give you a step-by-step Ayurvedic treatment protocol for Uterine Hypoplasia, the way an Ayurvedic physician (Vaidya) might approach it. This combines Ahara (diet), Vihara (lifestyle), Aushadhi (herbs/medicines), and Panchakarma (therapies).
Purva Karma (Preparatory Measures)
Before specific treatments, the body is prepared with gentle detox and nourishment:
-
Abhyanga (oil massage) with Bala Taila or Ksheerbala Taila → balances Vata, improves pelvic circulation.
-
Swedana (steam therapy) – mild fomentation after massage to open channels.
-
Nasya with medicated oil (e.g., Anu Taila, Ksheerbala Taila) – regulates hormones via the hypothalamic-pituitary axis.
Panchakarma Therapy (Main Ayurvedic Treatments)
-
Uttarbasti (main therapy for uterine nourishment)
-
Medicated ghee or oil (Phala Ghrita, Shatavari Taila) is administered into the uterus/cervix under strict supervision.
-
Directly nourishes uterine tissues, improves size, and enhances receptivity.
-
-
Basti (medicated enemas)
-
Yogabasti course using Dashmool Kwath, Ksheerbala Taila → balances Apana Vata, essential for reproductive health.
-
-
Virechana (mild purgation) if Pitta imbalance is present → clears toxins and regulates hormones.
Aushadhi (Medicines & Herbal Support)
Daily herbal medicines, often for 3–6 months:
-
Shatavari Kalpa – uterine tonic, estrogenic effect.
-
Ashokarishta – regulates menstruation, strengthens uterine walls.
-
Dashmoolarishta – balances Vata-Pitta, improves uterine nourishment.
-
Phala Ghrita (taken with warm milk) – improves fertility and uterine development.
-
Ashwagandha Churna – balances stress hormones, promotes tissue growth.
Ahara (Dietary Protocol)
-
Must-have foods:
-
Warm milk with Shatavari powder or Phala Ghrita.
-
Sesame seeds, almonds, walnuts, dates, figs, raisins, ghee, jaggery.
-
Green leafy vegetables, beetroot, carrots (iron + folate rich).
-
-
Spices: cumin, fenugreek, turmeric, ginger – aid digestion and absorption.
-
Avoid: junk food, excess caffeine, processed/packaged food, very spicy, cold, or stale foods.
Vihara (Lifestyle Protocol)
-
Yoga asanas (daily practice):
-
Baddha Konasana (Butterfly pose)
-
Setu Bandhasana (Bridge pose)
-
Bhujangasana (Cobra pose)
-
Paschimottanasana (Seated forward bend)
-
-
Pranayama:
-
Anulom Vilom (alternate nostril breathing)
-
Bhramari (humming bee breath) → calms stress, balances hormones.
-
-
Sleep: 7–8 hours daily (hormones are regulated during deep sleep).
-
Stress management: meditation, mantra chanting, journaling.
Rasayana (Rejuvenation Phase)
After the main treatment:
-
Long-term use of Shatavari, Ashwagandha, Guduchi, and Phala Ghrita in small doses.
-
Aims to rejuvenate the uterus and reproductive tissues.
Summary
-
Main treatment: Uttarbasti with Phala Ghrita/Shatavari Taila + Hormone-balancing Rasayana herbs.
-
Supportive: Panchakarma (Basti, Abhyanga, Nasya), Rasayana formulations.
-
Lifestyle: Yogasanas, pranayama, stress management.
-
Diet: Warm, nourishing foods with milk, ghee, nuts, and seeds.
This holistic protocol can gradually nourish the uterus, improve menstruation, and support fertility. It must be done under the supervision of an Ayurvedic doctor, especially for Uttarbasti and Panchakarma.
A timeline chart (Month 1 → Month 6) Uterine Hypoplasia
Let’s organize the Ayurvedic treatment for Uterine Hypoplasia into a clear step-by-step table. This will show the timeline, treatments, and focus in each phase.
| Phase | Duration | Main Therapies | Herbs / Medicines | Diet & Lifestyle | Focus / Goal |
|---|---|---|---|---|---|
| Purva Karma (Preparation) | 1–2 weeks | – Abhyanga (oil massage with Bala Taila/Ksheerbala Taila) – Swedana (mild steam) – Nasya (Anu Taila/Ksheerbala Taila) |
Non-specific (body prep stage) | – Light, warm food – Avoid heavy, cold foods – Begin gentle yoga (Baddha Konasana, Setu Bandhasana) |
Detox & prepare body for deeper therapy |
| Panchakarma (Main Therapy) | 2–4 weeks (under supervision) | – Uttarbasti with Phala Ghrita or Shatavari Taila (core therapy) – Basti (Yogabasti with Dashmool Kwath, Ksheerbala Taila) – Mild Virechana (if needed) |
Panchakarma-based oils/ghritas | – Continue nourishing foods (milk, ghee, nuts, sesame, dates) – Moderate yoga & pranayama |
Direct nourishment of the uterus, balance Vata-Pitta |
| Aushadhi (Herbal Therapy) | 3–6 months | – | – Shatavari Kalpa (uterine tonic) – Ashokarishta (regulates cycles) – Dashmoolarishta (balances Vata) – Phala Ghrita with warm milk – Ashwagandha Churna (stress & tissue support) |
– Rich diet: milk, ghee, almonds, figs, beetroot, carrots – Avoid junk/spicy food – Regular yoga & Anulom Vilom |
Stimulate uterine growth, regulate hormones, and restore menstruation |
| Rasayana (Rejuvenation & Maintenance) | Long term (after 6 months) | Light Panchakarma if needed | – Shatavari, Ashwagandha, Guduchi (low doses) – Phala Ghrita (occasional) |
– Follow Satmya Ahara (wholesome diet) – Stress-free lifestyle – Regular sleep & meditation |
Maintain uterine health, enhance fertility, prevent relapse |
Summary
-
Phase 1 (Prep): Gentle detox & preparation.
-
Phase 2 (Panchakarma): Core therapy with Uttarbasti & Basti → direct uterine nourishment.
-
Phase 3 (Herbs): Shatavari, Ashoka, Phala Ghrita for sustained growth & cycle regulation.
-
Phase 4 (Rasayana): Long-term rejuvenation for fertility & hormonal stability.

Conclusion
Uterine hypoplasia is a condition where the uterus remains underdeveloped due to hormonal, genetic, nutritional, or systemic factors, often leading to delayed puberty, menstrual irregularities, and fertility challenges. Early detection through clinical evaluation, imaging, and hormonal tests is crucial for effective management. Conventional treatment with hormone replacement therapy plays a central role, while supportive measures such as proper nutrition, lifestyle regulation, and stress management can enhance outcomes.
From an Ayurvedic perspective, uterine hypoplasia is addressed through a holistic approach involving Panchakarma therapies (especially Uttarbasti), Rasayana herbs like Shatavari and Ashoka, and a nourishing diet to strengthen reproductive tissues. Both modern and traditional approaches emphasize that timely intervention during adolescence offers the best chance for improving uterine growth, restoring menstrual health, and supporting fertility.
Ultimately, managing uterine hypoplasia requires a personalized, integrative approach that combines medical treatment, lifestyle care, and emotional support, helping affected women achieve better reproductive and overall health.
Frequently Asked Questions
1. What is uterine hypoplasia?
Uterine hypoplasia is a condition where the uterus is present but remains smaller and underdeveloped compared to the normal size for a woman’s age, often due to hormonal or developmental issues.
2. What causes uterine hypoplasia?
It can be caused by hormonal insufficiency (low estrogen, pituitary or ovarian dysfunction), genetic conditions (like Turner syndrome), malnutrition, chronic illness, or damage from radiation/chemotherapy during childhood.
3. What are the symptoms of uterine hypoplasia?
-
Absence of menstruation (amenorrhea) or irregular cycles.
-
Light or scanty periods (hypomenorrhea).
-
Delayed puberty or poor development of secondary sexual characteristics.
-
Infertility or repeated miscarriages.
-
In some cases, pelvic pain.
4. How is uterine hypoplasia diagnosed?
Diagnosis is made through:
-
Pelvic ultrasound/MRI – to measure uterine size.
-
Hormone tests – estrogen, FSH, LH, thyroid, prolactin.
-
Karyotyping – to check for genetic causes.
-
Clinical evaluation – puberty history, menstrual patterns, physical exam.
5. Can uterine hypoplasia be prevented?
Not always, but risk can be reduced with:
-
Good nutrition in childhood/adolescence.
-
Early detection of delayed puberty or menstrual irregularities.
-
Proper treatment of hormonal and chronic illnesses.
-
Avoiding unnecessary radiation or toxic exposures in young girls.
6. What are the modern medical treatments for uterine hypoplasia?
-
Hormone replacement therapy (HRT) with estrogen and progesterone.
-
Treating underlying endocrine or systemic conditions.
-
Fertility support with ovulation induction or IVF, and in severe cases, surrogacy.
7. Are there home remedies for uterine hypoplasia?
Home remedies cannot cure uterine hypoplasia, but they can support overall health:
-
Balanced diet (milk, nuts, sesame, leafy greens).
-
Moderate yoga and pranayama.
-
Stress management and proper sleep.
These should be combined with medical treatment.
8. What are the Ayurvedic treatments for uterine hypoplasia?
Ayurveda focuses on nourishing the uterus and balancing hormones:
-
Herbs: Shatavari, Ashoka, Lodhra, Ashwagandha.
-
Formulations: Ashokarishta, Dashmoolarishta, Phala Ghrita.
-
Panchakarma: Uttarbasti with medicated oils/ghrita, Basti, Abhyanga, Nasya.
-
Diet: Warm, nourishing foods with ghee, sesame, nuts, and milk.
9. Can women with uterine hypoplasia conceive?
-
Mild to moderate cases: With proper hormone therapy and fertility support, conception is possible.
-
Severe cases: Uterus may be too small to carry a pregnancy; IVF with surrogacy is usually advised.
10. What is the long-term outlook for uterine hypoplasia?
With early diagnosis and proper treatment, many women can achieve normal menstruation and improved fertility. In severe or genetic cases, fertility may be limited, but modern ART (assisted reproductive techniques) and holistic approaches (Ayurveda, nutrition, stress care) can greatly improve quality of life.
These FAQs cover definition, causes, symptoms, diagnosis, prevention, modern & Ayurvedic treatments, and fertility outlook.
Reference: https://en.wikipedia.org/wiki/Uterine_hypoplasia